Autologous T cell therapy targeting multiple antigens shows promise treating pancreatic cancer
A recent publication in Nature Medicine describes a novel immunotherapy targeting pancreatic cancer that has shown promising results in a first in-human phase 1/2 trial. The TACTOPS trial, which investigated the safety and clinical effects of autologous T cell therapy targeting multiple tumor antigens, was a collaboration between researchers at Baylor College of Medicine, the Dan L Duncan Comprehensive Cancer Center, the Center for Cell and Gene Therapy, Texas Children’s Hospital and Houston Methodist Hospital.
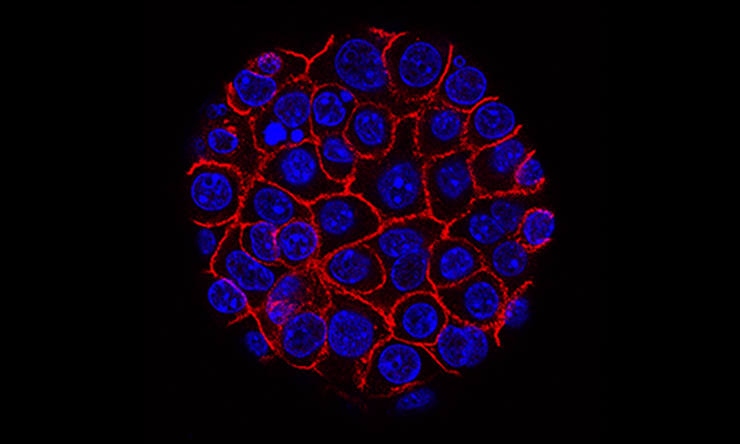
“We wanted to develop a targeted therapeutic that would hone the immune system on tumor-associated antigens (TAAs) that were present on malignant cells. We targeted five different antigens to deal with the polyclonal nature of the disease,” said co-corresponding author Dr. Ann Leen, professor of pediatrics – hematology and oncology in the Center for Cell and Gene Therapy.
“Pancreatic cancer doesn’t look as foreign to the immune system as other cancers do. This novel immunotherapy may help the immune system recognize and attack cancer cells in a way that other immunotherapies have not been able to do thus far,” said co-corresponding author Dr. Benjamin Musher, professor of medicine at Baylor and medical director of medical oncology at the Dan L Duncan Comprehensive Cancer Center.
Patients with pancreatic cancer were enrolled into one of three trial cohorts. Arm A included patients with advanced disease responding to first-line chemotherapy. Arm B included patients with metastatic disease who had progressed on first-line chemotherapy. Arm C included patients with surgically resectable disease. Each patient provided a blood sample, and individualized T cell therapy was manufactured at the Center for Cell and Gene Therapy. In total, 37 study participants received six monthly infusions of T cells.
Patients in arms A and C showed promising results, with 84.6% disease control rate in the group of patients responding to frontline chemotherapy (Arm A). Two out of nine patients in the those who underwent surgical resection (Arm C) remained disease-free more than five years after surgery. Researchers observed only 25% disease control in patients with refractory disease (Arm B). The therapy was extremely well-tolerated, with only one possibly treatment-related serious adverse side effect documented over all three cohorts.
Positive clinical outcomes correlated with functional T cell expansion and infused cell persistence in blood specimens collected during therapy compared to those collected at baseline. The investigators already are using the data from this study to refine their approach in preparation for the next trial, which may include T cell therapy alone or combined with other immune therapies.
“Nationwide, only 5% of pancreatic cancer patients enroll in clinical trials,” Musher said. “To improve pancreatic cancer outcomes meaningfully, we must explore all possible treatment options and enroll more patients in clinical trials. Studies like ours, which include robust correlative science, help us learn from successes and failures and facilitate further advances. They also provide patients with much-needed hope while helping them feel part of something larger than themselves.”
“The clinical and translational science expertise at Baylor within the Duncan Cancer Center and the Center for Cell and Gene Therapy enables our team to conduct complex trials that reach patients at different disease stages,” Leen said. “We could not accomplish this without strong collaboration between the lab and clinic, the excellent work of our regulatory team and top tier good manufacturing practices (GMP) facility.”
Drs. Spyridoula Vasileiou and Brandon G. Smaglo are co-first authors of this work with Musher. Other contributors include Catherine S. Robertson, Mengfen Wu, Tao Wang, Ayumi Watanabe, Manik Kuvalekar, Yovana Velazquez, Shamika Ketkar, Tamadar Al Doheyan, Penelope G. Papayanni, Aakash Shah, Natalia Lapteva, Bambi J. Grilley, George Van Buren, Premal D. Lulla, Helen E. Heslop, Cliona M. Rooney and Malcolm K. Brenner. All authors were affiliated with Baylor College of Medicine, the Center for Cell and Gene Therapy, Dan L Duncan Comprehensive Cancer Center, Texas Children’s Hospital and/or Houston Methodist Hospital when the study was conducted. See the publication for a full list of funding sources.







 Credit
Credit