What Are Emerging Infectious Diseases?
Emerging infectious diseases are infections that have recently appeared within a population or those whose incidence or geographic range is rapidly increasing or threatens to increase in the near future. Emerging infections can be caused by:
- Previously undetected or unknown infectious agents
- Known agents that have spread to new geographic locations or new populations
- Previously known agents whose role in specific diseases has previously gone unrecognized.
- Re-emergence of agents whose incidence of disease had significantly declined in the past, but whose incidence of disease has reappeared. This class of diseases is known as re-emerging infectious diseases.
The World Health Organization warned in its 2007 report that infectious diseases are emerging at a rate that has not been seen before. Since the 1970s, about 40 infectious diseases have been discovered, including SARS, MERS, Ebola, chikungunya, avian flu, swine flu, Zika and most recently COVID-19, caused by a new coronavirus, SARS-CoV-2.
With people traveling much more frequently and far greater distances than in the past, living in more densely populated areas, and coming into closer contact with wild animals, the potential for emerging infectious diseases to spread rapidly and cause global epidemics is a major concern.
Additionally, there is the potential for diseases to emerge as a result of deliberate introduction into human, animal, or plant populations for terrorist purposes, as discussed in the section on Bioterrorism Agents. These diseases include anthrax, smallpox, and tularemia.
Factors in the Emergence or Re-emergence of Infectious Diseases
There are many factors involved in the emergence of new infectious diseases or the re-emergence of “old” infectious diseases. Some result from natural processes such as the evolution of pathogens over time, but many are a result of human behavior and practices. Consider how the interaction between the human population and our environment has changed, especially in the last century. Factors that have contributed to these changes are population growth, migration from rural areas to cities, international air travel, poverty, wars, and destructive ecological changes due to economic development and land use.
For an emerging disease to become established at least two events have to occur – (1) the infectious agent has to be introduced into a vulnerable population and (2) the agent has to have the ability to spread readily from person-to-person and cause disease. The infection also has to be able to sustain itself within the population, that is more and more people continue to become infected.
Many emerging diseases arise when infectious agents in animals are passed to humans (referred to as zoonoses). As the human population expands in number and into new geographical regions, the possibility that humans will come into close contact with animal species that are potential hosts of an infectious agent increases. When that factor is combined with increases in human density and mobility, it is easy to see that this combination poses a serious threat to human health.
Climate change is increasingly becoming a concern as a factor in the emergence of infectious diseases. As Earth's climate warms and habitats are altered, diseases can spread into new geographic areas. For example, warming temperatures allow mosquitoes - and the diseases they transmit - to expand their range into regions where they previously have not been found.
A factor that is especially important in the re-emergence of diseases is antimicrobial resistance - the acquired resistance of pathogens to antimicrobial medications such as antibiotics. Bacteria, viruses, and other microorganisms can change over time and develop a resistance to the drugs used to treat diseases caused by the pathogens. Therefore, drugs that were effective in the past are no longer useful in controlling disease.
Another factor that can cause a disease to re-emerge is a decline in vaccine coverage, so that even when a safe and effective vaccine exists, a growing number of people choose not to become vaccinated. This has been a particular problem with the measles vaccine. Measles, a highly contagious and serious infection that was eliminated from the U.S. in 2000 and from the Western Hemisphere in 2016, has returned in certain areas due to an increase in the number of people opting to take nonmedical vaccine exemptions for reasons of personal and philosophical belief. This has been driven by an anti-vaccine movement that was founded largely on an invalid and discredited study that claimed a link between a vaccine against measles and autism. As a result of the decline in vaccine coverage, measles cases are highest by far this decade with more than 1,000 cases of measles reported in the U.S. in the first half of 2019.
Examples of How Diseases Emerge
Influenza (or flu) is an example of an emerging disease that is due to both natural and human factors. Influenza virus is infamous for its ability to change its genetic information. Large changes in the influenza virus can cause pandemics because the human immune system is not prepared to recognize and defend against the new variant. The chances of large genetic changes occurring and being passed into humans are increased when humans coexist in close proximity with agricultural animals such as chickens, ducks, and pigs. These animals are natural hosts of influenza virus and can act as mixing vessels to create novel versions of influenza that have not existed previously. Avian H5N1 influenza (or bird flu), which emerged more than a decade ago, has been limited to relatively rare instances of infection in humans who came into direct contact with diseased birds. The H5N1 virus is very deadly (more than half the cases have been fatal), but it has not acquired the ability to pass efficiently between humans. In contrast, the 2009 H1N1 influenza, which passed into humans from swine (pigs), transmitted easily from person to person and traveled quickly around the world as a result of human activity, particularly air travel. Fortunately, it was much less deadly than the H5N1 virus. Emergence of an influenza virus that is as deadly as the avian H5N1 virus and is spread between people as easily as the swine H1N1 virus would be a very serious threat to human health.
The case of the coronaviruses SARS-CoV, MERS-CoV, and SARS-CoV-2 (which cause the diseases SARS, MERS, and COVID-19 respectively), represents instances of how viruses can move from animals into humans, acquire the ability to spread from person to person and then, with great speed, reach around the globe as a result of air travel. These three viruses, which all cause severe respiratory illnesses and can be fatal, originated in bats and spilled over into the human population through close contact with an intermediate animal. SARS emerged in China in 2002, MERS in the Arabian Peninsula in 2015, and COVID-19 in Wuhan, China at the end of 2019. For SARS, an unprecedented global response halted the spread of the causative virus but not before 8000 people had been infected and 800 died. MERS has been largely contained but not before spreading to 27 countries and causing 2,500 infections and close to 900 deaths. The outcome of SARS-CoV-2, however, has been vastly more devastating. Aided by delayed and uncoordinated global responses, insufficient containment measures, and the fact that infected people can transmit the virus even in the absence of symptoms, the virus raged beyond the ability to control its spread and resulted in a worldwide pandemic that has lasted over a year and caused around three million deaths globally.
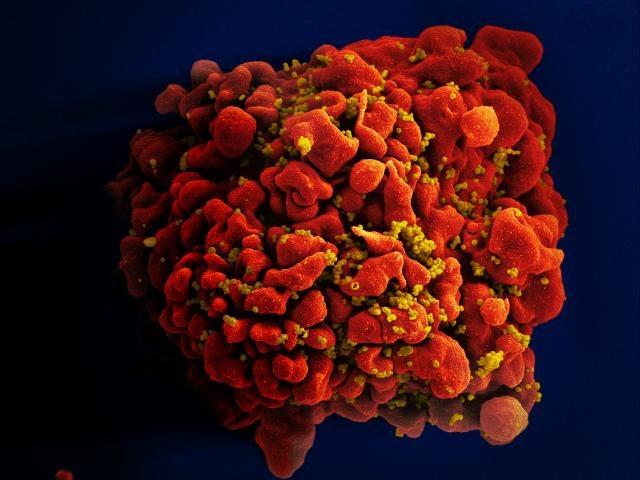
An example of an emerging infectious disease that can be attributed to human practices is HIV. It is thought that humans were first infected with HIV through close contact with chimpanzees, perhaps through bushmeat hunting, in isolated regions of Africa. It is likely that HIV then spread from rural regions into cities and then internationally through air travel. Further factors in human behavior, such as intravenous drug use, sexual transmission, and transfer of blood products before the disease was recognized, aided the rapid and extensive spread of HIV.
One instance of a tropical disease that has spread recently into new areas that may be due, at least in part, to changing climate is chikungunya. Chikungunya disease is caused by the chikungunya virus, a relative of the virus that causes Dengue fever. It is transmitted by the tiger mosquito, and in the past was confined to tropical regions around the Indian Ocean. In late summer of 2007, more than 100 residents of the town of Ravenna, Italy suffered from a mysterious disease that produced fever, exhaustion, and severe bone pain. The outbreak was eventually shown to be caused by chikungunya virus. By 2014, chikungunya outbreaks have been reported in countries in Europe, Asia, Africa, and the Americas (Caribbean and Central and South America). The virus arrived in the United States in the summer of 2014, although thus far local transmission of chikungunya virus has been limited to Florida and Texas. Although chikungunya virus does not usually cause a fatal disease, it serves as a warning that other, more devastating tropical diseases could follow. In fact, a more serious threat is the recently emergent Zika virus in the Americas which is associated with a birth defect known as microcephaly.
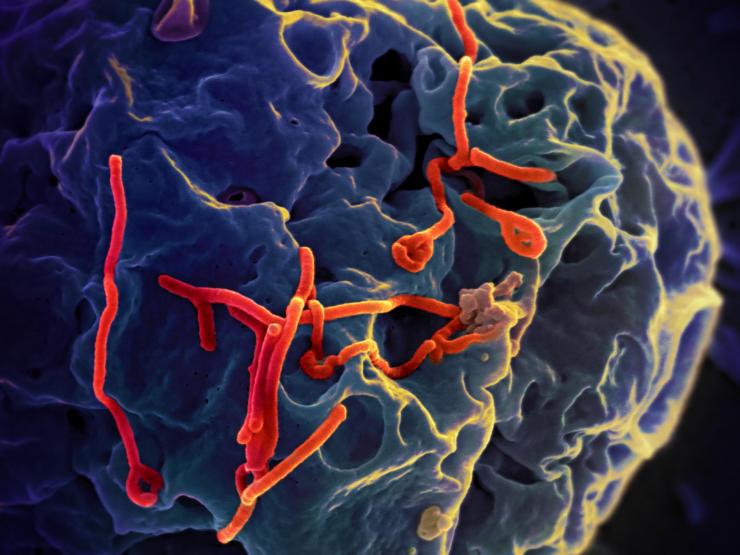
Finally, the Ebola virus epidemic that emerged in 2014 in West Africa illustrates how a virus that previously affected only small groups of people, perhaps a few hundred, can sweep rapidly through an area to affect tens of thousands, and become extremely difficult to contain. A combination of factors including high population densities, increased travel, closer contact with wild animals, weak health care systems, and a slow response led to the worst outbreak of Ebola the world has ever seen.
Research on Emerging Diseases
The development of vaccines and antimicrobial drugs and the remarkable eradication of smallpox had created hope that infectious diseases could be controlled or even eliminated. However, the current realization that infectious diseases continue to emerge and re-emerge (including the possibility of bioterrorism), underscores the challenges ahead in infectious disease research.
To help meet this challenge, research is ongoing in the Department of Molecular Virology and Microbiology at Baylor College of Medicine on a number of emerging and re-emerging diseases, including influenza, SARS-CoV-2, SARS and MERS, dengue, chikungunya, Zika, tuberculosis, and HIV/AIDS. This work encompasses both basic research in trying to understand more thoroughly how these agents cause disease and how the human immune system responds to these infections, as well as more directed research in developing and evaluating vaccines and other tools to prevent infection by these agents. In addition, scientists are studying mechanisms by which bacteria can acquire antibiotic resistance and ways to combat drug-resistant infections.
Glossary
Learn more about some of the technical terms found on our glossary of terms page.








 Credit
Credit