What is a Liver Transplantation?
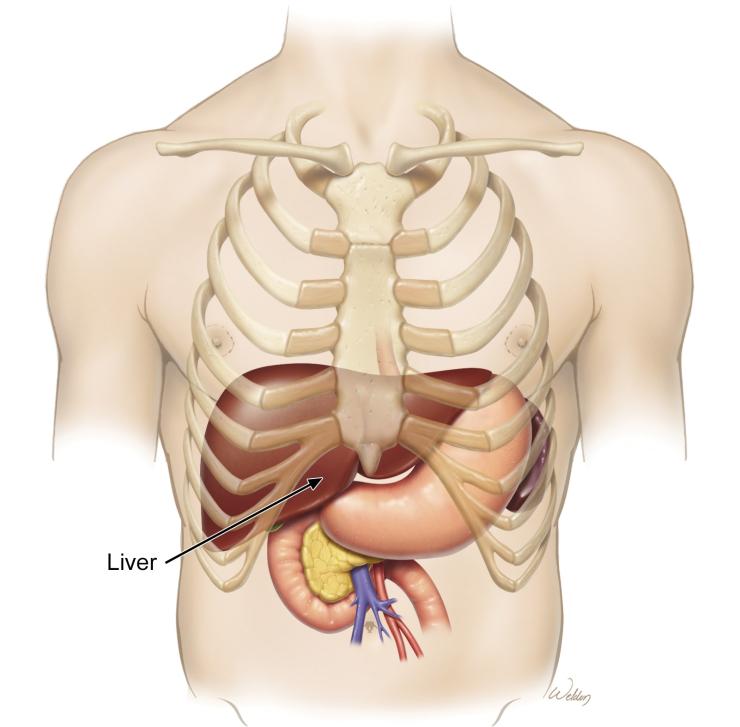
A liver transplant is a surgery to replace a diseased liver with a healthy liver from a donor. The liver is an important organ that helps with digestion, removing toxins from the blood, controlling bleeding and making proteins.
Why Do People Need Liver Transplants?
People need liver transplants when their liver is not working properly. This can happen due to both acute and chronic diseases like cirrhosis, liver cancer or hepatitis. A liver transplant can save lives by giving patients a new healthy liver, removing cancer and controlling the pressure in veins in the stomach and intestines.
Your Transplant Coordinator
A transplant coordinator is a healthcare professional who plays a crucial role in the organ transplant process. They serve as the main point of contact for patients, families and medical teams, ensuring a smooth and efficient transplant experience.
The coordinator will be your guide in the transplant listing and waiting processes, the transplant evaluation and all your lab work and testing and office visits. They will collaborate with all teams before and after surgery to be sure you receive comprehensive care. You’ll receive a large amount of detailed information from them on all these processes. Please be sure to read through it with your loved ones to make your transplant journey as smooth as possible.
Before Surgery
Evaluation: Your healthcare team will evaluate you to see if you’re a good candidate for a liver transplant. This includes blood tests, imaging tests like CT scans or MRIs and discussions about your medical and social history. They’ll also evaluate your social support, ability to obtain necessary medications and willingness to follow instructions closely.
Waiting List: If you’re approved, you’ll be placed on a waiting list for a liver from a donor based on how urgent your need is. This can take some time, depending on your blood type and how urgent your need is.
Preparing for Surgery: You will need to discontinue any alcohol and tobacco use. You will be given an exercise program to follow in preparation for your transplant.
Surgery Day: Once a liver is available, you’ll need to go to the hospital quickly. You’ll receive instructions on what to eat and drink before the surgery.
During Surgery
- You will be given general anesthesia, so you will be completely asleep.
- Through an IV, you will receive fluids and other medicine like antibiotics during the surgery.
- After you are completely asleep, a breathing tube will be placed into your windpipe through your mouth to help you breathe. During the surgery this tube will be connected to a breathing machine.
- You will have a tube placed into your bladder to drain your urine. This will be removed once you can get up and move around comfortably after surgery.
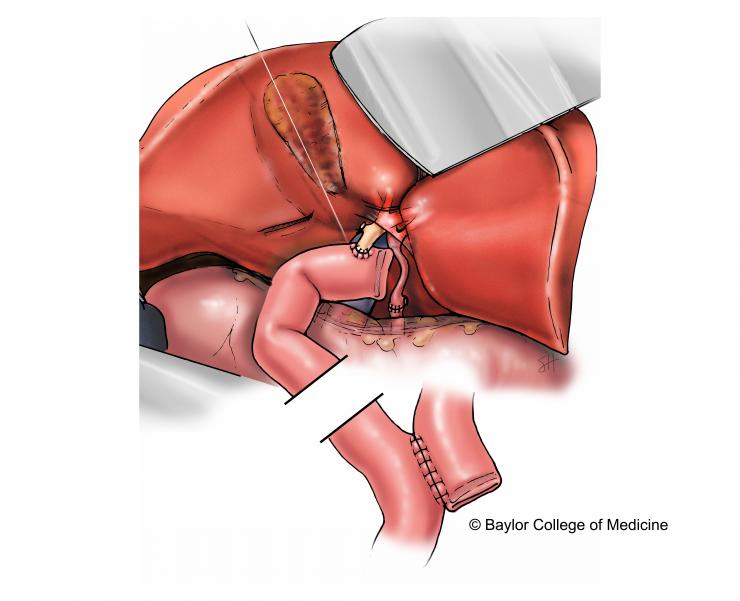
- Incision: The surgeon will make an incision on your abdomen to reach the liver.
- Removing the diseased liver: The surgeon will carefully remove your damaged liver.
- Placing the new liver: The new liver is then placed inside your body. The surgeon will connect the blood vessels and bile ducts from the new liver to your body.
- Closing the incision: The surgeon will close the incision with sutures and staples.
After Surgery
Recovery - What to Expect
After surgery, your anesthesiology and surgery team will accompany you to the Cardiovascular Critical Care (CVCC) unit. The next day, you will be moved to the surgical ICU, where you’ll stay for at least two to three days for close monitoring. After that, you’ll be moved to the transplant floor for the rest of your stay.
You’ll likely stay in the hospital for at least 14 days after your transplant. Doctors and nurses will monitor your recovery, checking to make sure the new liver is working properly and that you are recovering appropriately.
Breathing tube
For your safety, your breathing tube will still be in place in your mouth when you wake up. This can be frightening, because you won’t be able to speak and it may feel uncomfortable. Try to relax, breathe normally and let the breathing machine (ventilator) do the work and breathe for you. Your doctor will have the tube removed once you can breathe well on your own.
After the breathing tube is removed, you may feel groggy and disoriented. If you feel chilly or like your stomach is upset, ask your nurse to help you get comfortable.
Other tubes and wires
You will notice the following:
- EKG wires on your chest to record the activity of your heart
- A monitor on your finger to measure the oxygen in your blood
- IV lines for pain medication and fluids, and a special IV in your neck to measure heart function
- Catheter in your bladder
- Nasogastric (NG) tube in your nose to allow your stomach to rest
- Possibly another smaller feeding in your nose for extra nutrition
- Possibly straps to restrain your arms or pads on your hands (if you were pulling at your tubes and cords while waking up)
Follow-Up Care
Your transplant coordinator will set up all your clinic visits and tests, such as lab work. You will come back to the transplant clinic for follow-up visits once a week for the first month after leaving the hospital. Your comprehensive care team will see you that day to make sure you are recovering well. This will include your transplant coordinator, your surgeon, a pharmacist and possibly a nurse practitioner.
You will also need to have labs drawn two times every week for the first month after going home. On the morning before your lab work, you may take ALL of your medications EXCEPT for immunosuppression medications (Prograf/sirolimus). You should take these medications immediately after your labs have been drawn. Regular check-ups with your doctor will be necessary to ensure your liver stays healthy. You’ll also need to follow a healthy lifestyle, including eating a balanced diet, exercising and avoiding alcohol and tobacco use.








 Credit
Credit