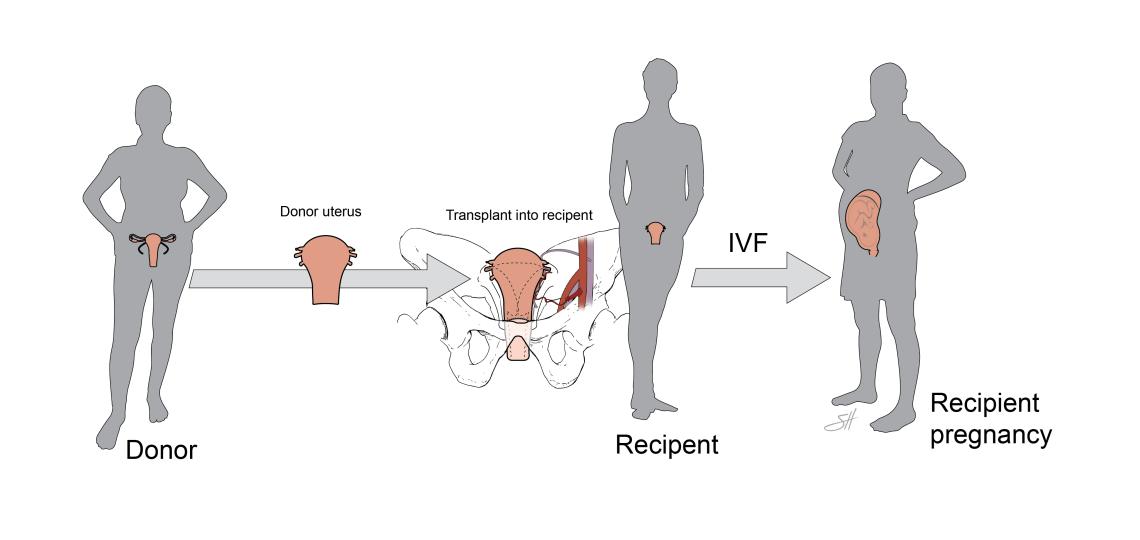
Uterine transplantation is an innovative medical procedure that involves the transplantation of a healthy uterus into the body of an individual who is unable to conceive due to absolute uterine factor infertility (AUFI). AUFI can be caused by a variety of conditions, such as congenital absence of the uterus (Mayer-Rokitansky-Küster-Hauser syndrome), damage from infection or surgeries, or other uterine anomalies. The goal of a uterine transplant is to enable the recipient to become pregnant and carry a pregnancy to term.
The process of a uterine transplant is complex and involves multiple stages:
Evaluation and Selection
Potential recipients undergo a thorough evaluation to ensure they are good candidates for the procedure. This includes psychological assessment, fertility evaluation, and overall health screening to manage risks. Likewise, donors, who may either be living or deceased, are screened for compatibility and the health of the uterus.
Surgical Procedure
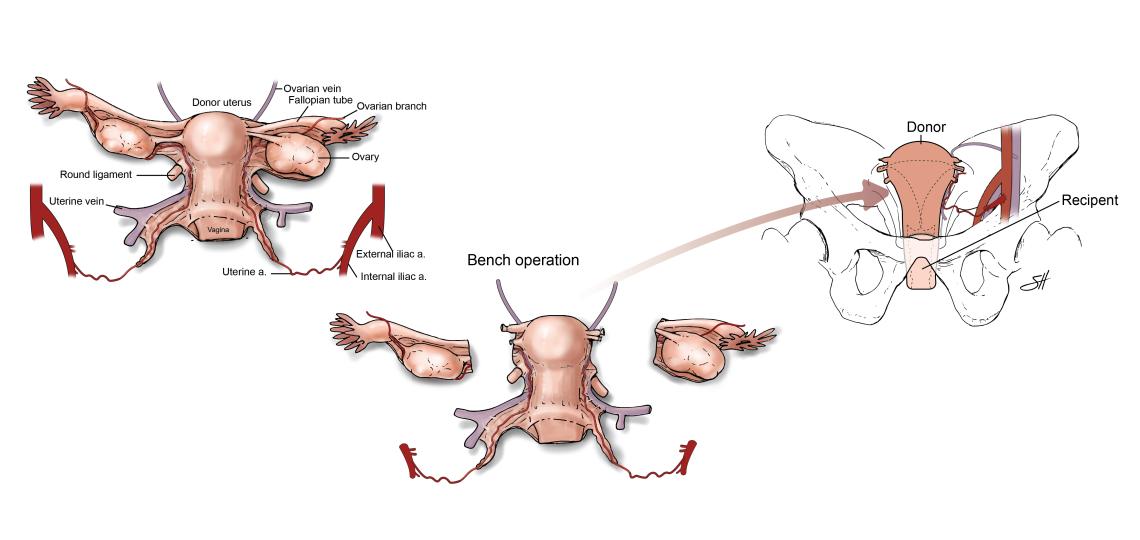
Uterine transplant surgery is intricate and can last several hours. For a living donor, the uterus is carefully removed preserving vital blood vessels and tissues. For a deceased donor, the process must occur soon after the donor's death to maintain the organ's viability.
Once the uterus is procured, the recipient undergoes surgery to implant the uterus into the pelvic region. Surgeons connect the uterus to the recipient's blood vessels and create a connection to the recipient's vagina. The success of the surgery is dependent on the establishment of a blood supply to the new uterus.
Recovery and Monitoring
Post-transplant, the recipient is closely monitored for signs of organ rejection or complications. Immunosuppressive drugs are administered to help prevent organ rejection. The patient and medical team must be vigilant for any signs of infection or complications due to these medications.
Fertility Treatment
Once the transplanted uterus is healed and functioning properly, typically after a year, the recipient can begin fertility treatments. This involves in vitro fertilization (IVF), since the fallopian tubes are not connected to the transplanted uterus. Embryos created before the transplant are transferred to the uterus with the hope of achieving pregnancy.
Pregnancy and Childbirth
Pregnancies through uterine transplants are considered high-risk and require close medical supervision. If a pregnancy is achieved, the baby must be delivered via cesarean section to avoid complications with the transplanted uterus.
After the birth of a child, the patient and her care team will discuss the feasibility, safety, and risks of proceeding with subsequent pregnancies. Once the uterus is no longer necessary, it is removed. The removal of the uterus allows the recipient to stop taking immunosuppressive drugs.
Uterine transplants are rare but becoming a viable treatment option for absolute uterine factor infertility. They represent a significant advancement in reproductive medicine, offering hope to those with AUFI who wish to experience pregnancy. The long-term health implications for both donor and recipient and the complexity of the procedure require a multidisciplinary approach from a dedicated team of specialists. As research and techniques improve, uterine transplants may become more accessible, providing more individuals the opportunity to carry a pregnancy.








 Credit
Credit