The Agent
Although tuberculosis (TB) is an ancient disease, it is still a major killer today. In 2006, 1.7 million people died of the disease worldwide and more than nine million new cases of TB emerged. TB is contagious and is spread from person to person through the air, for example, as when an infected person coughs or sneezes, and the bacteria are inhaled by another person nearby. TB usually affects the lungs, although it can also affect other parts of the body, such as the brain, kidney, or spine. Symptoms include general weakness, fever, night sweats, prolonged coughing (sometimes with coughing up of blood), and chest pain.
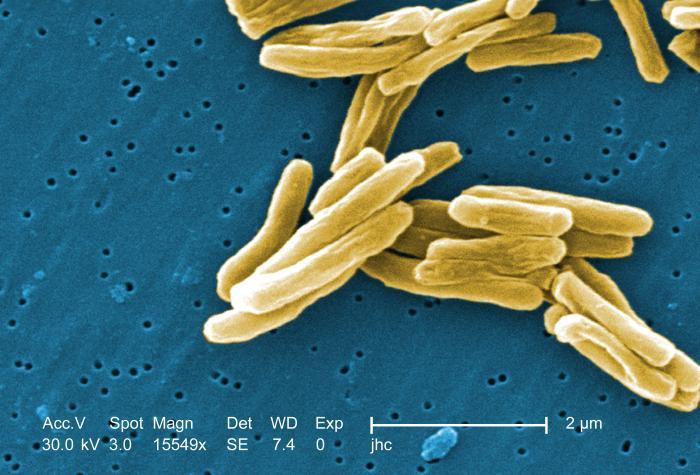
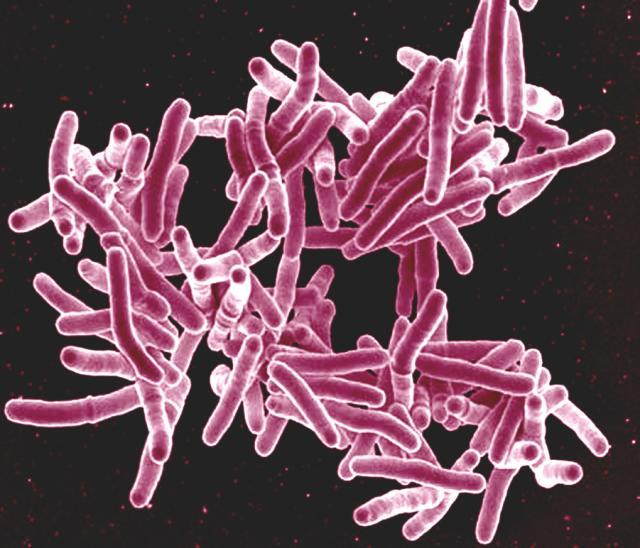
TB is caused by the bacterium Mycobacterium tuberculosis. This bacterium, also known as Koch’s bacillus, was discovered by Dr. Robert Koch in 1882. The TB bacterium is small, rod-shaped, and grows slowly. It is found only in people and not in other living organisms or in soil. It requires oxygen to survive.
One-third of the world’s population is infected with the TB bacterium. Most of these people have latent TB infections, meaning that TB bacteria are present in their bodies, but the bacteria are not active; these individuals do not have active TB disease and are not contagious. However, one in ten people with latent TB will develop active TB disease at some point in their lives. Active TB occurs when the TB bacteria replicate within a person’s body and destroy tissue in the body, usually causing symptoms of TB disease. Active TB is most likely to develop in people with weakened immune systems. In the United States, an estimated 10 to 15 million people have latent TB; nearly 14,000 cases of active TB were reported by the Centers for Disease Control and Prevention in 2006. Foreign-born individuals have a much higher frequency of TB infection than people born in the United States, due to the higher prevalence of TB in other parts of the world, especially South-East Asia and Africa.
TB can usually be treated and cured with antibiotics, if treated promptly and correctly. However, the emergence of new forms of TB bacteria that are resistant to some antibiotics commonly used to treat TB has made treatment more difficult. Multidrug-resistant TB (MDR TB) is resistant to the two best antibiotics used against TB, isoniazid and rifampin, which are considered first-line drugs. MDR TB patients must undergo up to two years of multidrug treatment with second-line antibiotics. An even more dangerous form of TB, known as extensively drug-resistant TB (XDR TB), has arisen that is resistant to the first-line antibiotics and at least some of the second-line antibiotics. Treatment of people infected with XDR TB is challenging and may not be very effective.
Drug-resistant forms of TB emerge when antibiotics are not used appropriately. When a patient fails to complete a full course of antibiotics, a healthcare worker prescribes an incorrect treatment regimen, or the drug supply is unreliable, drug-resistant forms of TB can emerge. An individual may acquire MDR or XDR TB directly from another person infected with one of these forms if they inhale the drug-resistant TB bacteria. Alternatively, when a person is undergoing treatment for active TB and fails to properly comply with the course of treatment, the TB bacteria may have a chance to evolve into a drug-resistant form within their body.
The Problem
Every second, someone in the world becomes newly infected with the TB bacterium. It is estimated that nearly one billion people worldwide will become infected with the TB bacterium between now and 2020, and that over 150 million will become sick and 36 million will die.
Antibiotic resistance is significant cause of the resurgence in tuberculosis, and the emergence of drug-resistant forms of TB presents a serious challenge to the global healthcare community. While drug-resistant TB is usually treatable, anti-drug regimens using second-line antibiotics are generally much lengthier, costlier, and may produce more severe adverse effects than treatment with first-line antibiotics. Outcomes may also be more negative especially for patients with XDR TB, which fortunately is still quite rare. In a study of patients treated between 1993 and 2002, patients with XDR TB were 64 percent more likely to die than patients with MDR TB.
Another important reason for the increase in global TB cases – and a significant obstacle to controlling TB – is the AIDS epidemic. One third of the increase in TB cases is attributable to the AIDS epidemic. Infection with both the AIDS virus and the TB bacterium is a deadly combination. HIV, the virus that causes AIDS, suppresses the immune system. Because active TB is much more likely to occur among people with weakened immune systems, HIV-positive individuals who have a latent TB infection are much more likely to develop active TB than people who are not infected with HIV. In fact, TB is the leading cause of death among HIV-infected individuals. MDR TB is especially dangerous in a person with HIV infection, and these people generally have a more rapid course of disease and a higher mortality rate. Therefore, not only are HIV-positive people more likely to develop active TB, they are also more likely to die of TB. The World Health Organization estimates that over 11 million people worldwide are dually infected.
Currently, there is no vaccine proven to prevent lung disease caused by the TB bacterium. Although a vaccine against TB called BCG (Bacillus Calmette-Guérin) exists and is widely used in many countries with a high prevalence of TB, it is not generally recommended for use in the United States for several reasons. First, there is insufficient evidence that BCG is consistently effective in preventing adult pulmonary TB, the most common form of the disease (although it may be useful in preventing other forms of TB in children). Furthermore, the vaccine is associated with a low risk of infection with the TB bacterium, which makes it unsuitable for people with weakened immune systems, such as HIV-positive individuals. The BCG vaccine can also produce a false positive result on a tuberculin skin test, which makes it more difficult to monitor the population for TB prevalence. Clearly, a more effective vaccine is needed.
TB is a disease that seemed manageable several decades ago, but a combination of factors – principally the emergence of drug-resistant forms and the AIDS epidemic - has led to a resurgence of TB.
The Research
It is important to monitor the prevalence of TB – and especially drug-resistant TB – within the population. Hana El Sahly, M.D. of the Department of Molecular Virology and Microbiology (MVM) and her colleagues at Baylor College of Medicine have studied a group of patients infected with drug-sensitive and drug-resistant TB over the course of about five years. Among these patients from the Houston area, they found a steady, low-level incidence of drug-resistant TB that disproportionately affected certain subpopulations. Those that were more likely to have drug-resistant TB included HIV-positive individuals, people of Hispanic or Asian ethnicity, and those with a history of past TB. There were 15 patients in their study who acquired drug resistance while on therapy; these patients were also more likely to be HIV-positive or of Asian ethnicity.
Dr. El Sahly has also been involved in a study that investigated whether TB isolated from patients in the Houston area is susceptible to moxifloxacin, one of a class of antibiotics called quinolones that are used as second-line anti-TB drugs. Patient samples were analyzed for reduced susceptibility to moxifloxacin and other quinolone antibiotics, as well as first-line antibiotics. They further examined the samples to identify mutations in genes associated with reduced susceptibility to the quinolone antibiotics. They found that there is a low incidence of moxifloxacin-resistant TB in this patient group, and it is associated with MDR-TB. Previous exposure to quinolones was common among these patients. This work should help in the design of better treatment regimens and provides a basis for further monitoring and research on TB drug resistance.
For More Information
- Basic information about TB from the CDC
- Information about drug-resistant TB from the CDC
- Information about TB, including research, from the National Institutes of Health
- Information about TB including estimated global and regional incidence from the World Health Organization
- Information about TB from the American Lung Association
Glossary
Learn more about some of the technical terms found on this page by visiting our glossary of terms.








 Credit
Credit