The Agent
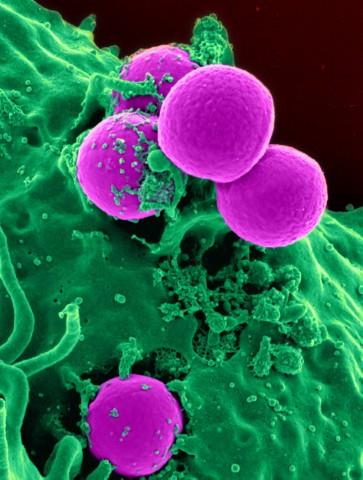
Staphylococcus aureus, often referred to as “staph”, is a common type of bacterium that is found in about 25 to 30 percent of healthy people, primarily on the skin or in the nose. Most of these individuals are colonized by the staph bacteria, meaning that the bacteria are present but are not causing disease. Some people become infected with staph bacteria indicating that the bacteria are present and cause disease. Although staph bacteria do not usually cause infection, they can bring about disease if they penetrate through a break in the skin or through mucous membranes.
Staph bacteria are one of the most common causes of skin infections and sometimes produce relatively minor skin infections such as pimples and boils. However, they can cause more serious illnesses such as surgical wound infections, bloodstream infections, bone infections, and pneumonia.
In the past few decades, a more dangerous form of staph has emerged. This form is known as methicillin-resistant Staphylococcus aureus and is usually referred to by the acronym MRSA. What sets MRSA apart is that it is resistant to an entire class of antibiotics called beta-lactams. This group of antibiotics includes methicillin, and the more commonly prescribed penicillin, amoxicillin, and oxacillin among others.
MRSA is categorized by the setting in which it is acquired. The first type, healthcare-acquired MRSA (HA-MRSA), has been recognized since the 1960s. Strains of staph were identified in patients in hospital and healthcare facilities that were resistant to methicillin (resistance to penicillin had occurred even earlier). The incidence of this infection has been increasing over time, with patients who have had surgery, medical devices implanted, or weakened immune systems being particularly at risk.
Of greater concern is a second type of MRSA which appeared in the 1990s and is known as community-acquired MRSA (CA-MRSA). CA-MRSA occurs outside of hospital settings and usually manifests itself as a skin infection in an otherwise healthy individual. CA-MRSA can develop into a more serious, life-threatening illness. CA-MRSA tends to occur under conditions where people are in prolonged physical proximity, such as in childcare and long-term care facilities, and in soldiers, prisoners, athletes involved in skin-to-skin contact sports such as wrestling, and in individuals sharing personal items such as towels. Unlike HA-MRSA, the source of infection for CA-MRSA is often difficult to identify.
Infection
CA-MRSA usually enters the body though a cut or scrape. The first sign of infection is commonly described as resembling a spider bite – a spot on the skin that is red, swollen, and painful. The site may produce pus. Infrequently, CA-MRSA infection can progress to a more serious disease, such as bloodstream infection or pneumonia. CA-MRSA can, in rare cases, lead to death. Highly publicized accounts of the deaths of at least three students from CA-MRSA in late 2007 prompted concern among students, parents, and school officials. The best defense against MRSA is to maintain good hygiene, including frequent and thorough hand washing, and to avoid the sharing of personal care items.
HA-MRSA and CA-MRSA differ at the genetic level and have distinct biologic properties. These differences suggest that CA-MRSA strains may spread more easily from person to person or cause more skin disease than HA-MRSA. At least three different strains of staph that cause CA-MRSA infections have been identified in the United States. Scientists are working towards understanding the differences between these strains and determining why certain people become infected and seriously ill.
The Problem
The incidence of disease caused by MRSA bacteria is increasing worldwide. Thirty years ago, MRSA accounted for 2 percent of staph infections. By 2003, 64 percent of staph infections were caused by MRSA. According to a report by the Centers for Disease Control and Prevention (CDC) in the United States in 2005, more 94,000 people developed life-threatening infections caused by MRSA; nearly 19,000 people died during hospital stays related to these MRSA infections. The majority of MRSA cases, 85 percent, were associated with healthcare facilities, while approximately 14 percent occurred in individuals with no known exposure to healthcare.
The staph bacterium continues to evolve and is beginning to show resistance to additional antibiotics. In 2002 the first staph strains were found that are resistant to vancomycin, an antibiotic that is one of the few available treatments used as a last resort against MRSA. Although vancomycin-resistant staph strains are currently still quite rare, it is feared that these strains will become more widespread over time and further reduce the limited number of antibiotics that are effective against MRSA.
The rising problem of resistance of staph bacteria to methicillin and other antibiotics is part of a larger issue that greatly concerns healthcare professionals. The emergence of antimicrobial-resistant organisms is making it more difficult to treat a variety of infectious diseases. Besides MRSA, the treatment of other diseases complicated by drug resistance include HIV, tuberculosis, influenza, and malaria.
Drug resistance occurs because microbes, such as staph bacteria, need to reproduce to ensure their survival. When this ability is threatened, as when they are exposed to antibiotics, microbes adapt and evolve to overcome the block to their reproduction. This can occur naturally, and microbes become genetically altered in ways which allow them to survive in the presence of antimicrobial drugs. However, drug resistance adaptations can be accelerated by human actions, particularly by the overuse and inappropriate use of antibiotics. The escalating use of antimicrobials in humans, animals, and agriculture is increasing the problem of drug resistance.
The consequences of antimicrobial resistance pose a significant concern to scientists and medical professionals. Infection with drug-resistant organisms can lead to increased and longer hospital stays, more complicated treatment, more deaths, and higher healthcare costs.
The Research
Surveillance of drug-resistant strains of MRSA
As strains of staph continue to adapt and change over time, it is critical for healthcare workers to track these changes. They need to know which strains are present within a community at any point in time, to which antibiotics the strains are resistant, and the severity of disease caused by the circulating strains. Two researchers affiliated with the Department of Molecular Virology Microbiology at Baylor College of Medicine, Drs. Edward Mason and James Versalovic and their colleagues have been conducting surveillance of both HA-MRSA and CA-MRSA in pediatric patients at Texas Children’s Hospital beginning in 2001. By analyzing strains isolated from these patients, the scientists have found that CA-MRSA accounts for an increasing percentage and number of infections. This information can help doctors select the optimal antibiotic treatment for infected patients.
Genetics changes in MRSA
Scientists would further like to understand the genetic changes in MRSA that allow the bacterium to cause serious illness in otherwise healthy individuals. To begin to answer this question, MVM scientists and others at Baylor College of Medicine initiated a project to obtain the DNA sequence of a strain of CA-MRSA called USA300. They chose the USA300 strain, one of two strains that cause the majority of CA-MRSA cases, because it has emerged as the predominant strain causing skin infections, as well as more serious infections, in both pediatric and adult patients in many states. Before 2000 this strain was rarely found in the community; today it accounts for 70 percent of CA-MRSA patients at Texas Children’s Hospital. Another reason for the interest in the USA300 strain is that it appears to be more virulent than other strains.
Drs. Sarah Highlander and Joseph Petrosino and colleagues at the Baylor Human Genome Sequencing Center sequenced the genome of this MRSA-resistant strain from a pediatric patient along with a community-associated staph strain that is susceptible to methicillin. They then compared the DNA sequences. They also compared the DNA sequence of these strains with the previously published staph genomes of isolates obtained elsewhere.
Based on the results of this analysis, the scientists concluded that the USA300 strain that they sequenced was very similar to other staph strains. This suggests that the increased virulence of the USA300 strain is due to subtle genetic changes within its genome. One intriguing finding of their study is that the bacterium has picked up a plasmid that contains a gene that confers resistance to bacitracin, an antibiotic commonly found in over-the-counter skin ointments.
With the genetic information describing USA300 in hand, the scientists can now zoom in on the regions that differ from other strains to pinpoint genes that may account for the ability of USA300 to cause serious illness in some people.
Mechanism of resistance to methicillin
Beta-lactam antibiotics are the most widely used class of drugs for the treatment of bacterial infections. They include penicillin and its derivatives, such as methicillin and amoxicillin. The beta-lactam ring portion of the antibiotic targets the penicillin-binding proteins (PBP), found in the bacterial cell membrane, which function in the synthesis of the cell wall. Binding of the antibiotic to the PBPs prevents the PBPs from performing their essential role and results in the death of the bacterial cell.
Dr. Timothy Palzkill, professor of Pharmacology and Chemical Biology and Molecular Virology and Microbiology, and his research team have been studying mechanisms of resistance to methicillin and other beta-lactam antibiotics. Gram-positive bacteria acquire resistance to beta-lactam antibiotics through the production of a protein called PBP2a, which is able to avoid the inhibitory effects of the antibiotics. This is the mechanism by which MRSA is able to persist despite treatment with multiple beta-lactam antibiotics.
Dr. Palzkill and coworkers conducted a study in which they found that the protein BLIP-II was able to weakly bind and inhibit PBP2a, making it susceptible to beta-lactam antibiotics. They are continuing this line of research by searching for mutations that increase the affinity of BLIP-II to PBP2a.
More Information
- Information about symptoms, prevention, and treatment of MRSA from the CDC as well as specific information for athletes, healthcare providers, and school officials
- Information about MRSA from the National Institutes of Health
- More information about MRSA from the National Institutes of Health
- MRSA information from the Texas Department of State Health Services
Glossary
Learn more about some of the technical terms found on this page by visiting our glossary of terms.








 Credit
Credit