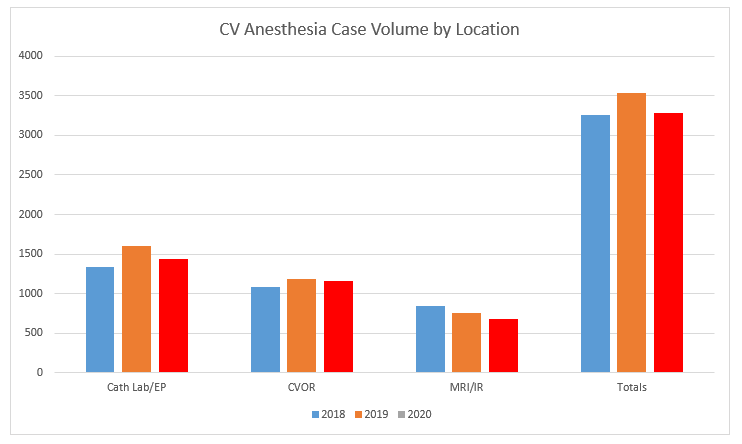
We believe that our clinical volume and complexity are one of the greatest strengths of our program. Reflecting this volume are our anesthetizing locations, which include:
- 4 cardiovascular operating rooms
- 3 cardiac catheterization labs
- 1 electrophysiology lab
- A procedure room suite
- CT
- MRI
- Interventional radiology
At all of these sites, our fellows are paired 1:1 with an attending anesthesiologist, thereby increasing the fellows’ procedural experience as well as fellow-level directed learning. In our operating rooms, fellows routinely place the necessary central and arterial lines.
Below are data demonstrating our case volume as a system as well as fellows’ case numbers over recent years. The end-result of our clinical experience is that our fellows are well-prepared to manage any patient presenting for any procedure.
| Case Type | Total |
|---|---|
| Stage 1 Palliation (Norwood) | 19 |
| Bidirectional Cavopulmonary Anastomosis (BDG) | 36 |
| Fontan | 26 |
| Arterial switch (dTGA and dTGA/VSD) | 14 |
| Truncus arteriosus | 9 |
| Tetralogy of Fallot | 27 |
| Complete atrioventricular septal defect | 18 |
| Coarctation of the aorta | 21 |
| Heart transplant | 24 |
| Lung transplant | 5 |
| VAD | 26 |
| ECMO as primary procedure (not post-cardiotomy) | 62 |
| Adult congenital | 55 |
Procedure | Average (range) |
|---|---|
| Fellow as sole trainee, total bypass cases | 113 (101-136) |
| Stage 1 Palliation (Norwood) | 8 (6-10) |
| Bidirectional Cavopulmonary Anastomosis (BDG) | 8 (6-10) |
| Fontan | 7 (5-10) |
| Arterial switch | 6 (5-9) |
| Other neonatal procedures | 15 (7-23) |
| Coarctation of the aorta | 6 (4-13) |
| Cardiac or lung transplant | 6 (6-7) |
| Placement of circulatory assist device | 13 (6-19) |
| Diagnostic catheterization procedures | 38 (25-55) |
| Interventional catheterization procedures | 41 (39-45) |
| Central venous catheterization | 104 (85-136) |
| Arterial line placement | 117 (104-143) |