What Is Moyamoya Disease?
Moyamoya disease is a rare, progressive cerebrovascular disorder caused by the shrinking of major brain blood vessels resulting in decreased blood flow to certain brain regions and eventually can lead to stroke. The term moyamoya was coined by the Japanese physicians who discovered it and means “puff of smoke” which describes the appearance of the network of tiny vessels that form at the base of the brain in moyamoya (Figure 1a). Although it was first discovered in Japan and is more common in Asian countries, the disorder has been found in individuals throughout the world including the United States. Moyamoya most commonly affects children and young adults and there is currently no known medical cure, but surgery to increase blood flow to the brain is an effective option.
The cerebrovascular neurosurgeons at Baylor Medicine and Baylor St. Luke’s Medical Center in Houston, Texas, specialize in the diagnosis and treatment of moyamoya disease and other brain blood vessel disorders. Located in the heart of Houston’s renowned Texas Medical Center, our neurosurgeons are one of the rare groups in the country with expertise in the diagnosis and treatment of moyamoya disease. Each patient is different and our doctors provide expertise managing this disorder.
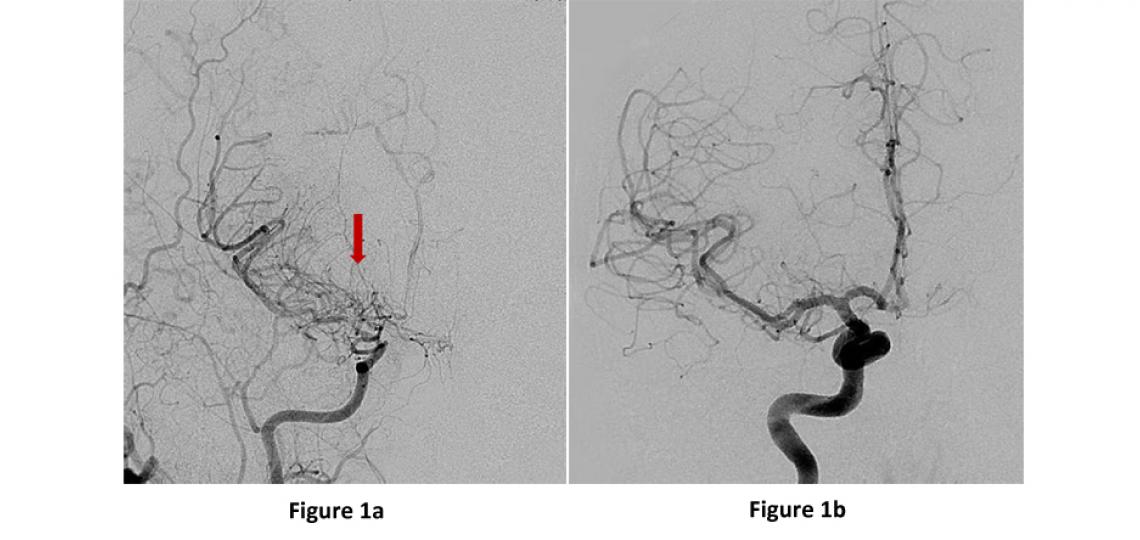
Figure 1a: AP or front view of a brain angiogram showing the right internal carotid artery narrowing into the small tangles of moyamoya “puff of smoke” vessels (red arrow). Figure 1b: A normal angiogram for comparison.
Symptoms
Common symptoms of moyamoya disease include:
- Weakness or numbness of the face, arm or leg
- Difficulty speaking or comprehending speech
- Visual changes
- Headaches
- Seizures
- Balance difficulties
- Transient ischemic attacks (TIAs) or stroke-like symptoms that come and go
Diagnosis
If moyamoya disease is suspected, it is important to make a diagnosis and consult with a specialist quickly to prevent worsening of the disease. Based on the patient’s symptoms, the physician may order one or all of these tests. All of these tests are often needed before making a decision about surgery.
- Magnetic resonance imaging (MRI)
- Cerebral angiogram
- Perfusion scans (MRI or CT perfusion)
- Neuropsychological assessment
Outcome of Untreated Moyamoya Disease
Without surgery, most patients with moyamoya disease will experience slowly narrowing brain arteries, decreasing brain blood flow, and over time develop ischemic strokes, mental decline and even potentially death from a brain bleed.
Treatment
Currently, there is no medical treatment to reverse moyamoya disease, and surgery is the only disease altering treatment. In patients with favorable medical histories and imaging studies, surgery for moyamoya disease can slow and even stop the disease from worsening by increasing blood flow to the brain. Which type of surgery is the best varies, depending on the individual patient and their unique version of moyamoya and vessel anatomy. There are two major types of surgeries to increase blood flow to the brain:
- Direct revascularization
- Indirect revascularization
Direct Revascularization
Direct revascularization (also called STA-MCA bypass or EC-IC bypass) is an open brain surgery that uses a blood vessel from the skin on the side of the head (superficial temporal artery or STA), cuts it and directly sutures the cut end to a recipient vessel on the surface of the brain (middle cerebral artery or MCA) (Figure 2a-b). This surgery provides an immediate increase in brain blood flow by “bypassing” the blocked vessel at the base of the brain and creating a new blood flow pathway into the brain beyond the blockage. Over time, the sutured vessel continues to grow and supply more and more blood flow to the brain.
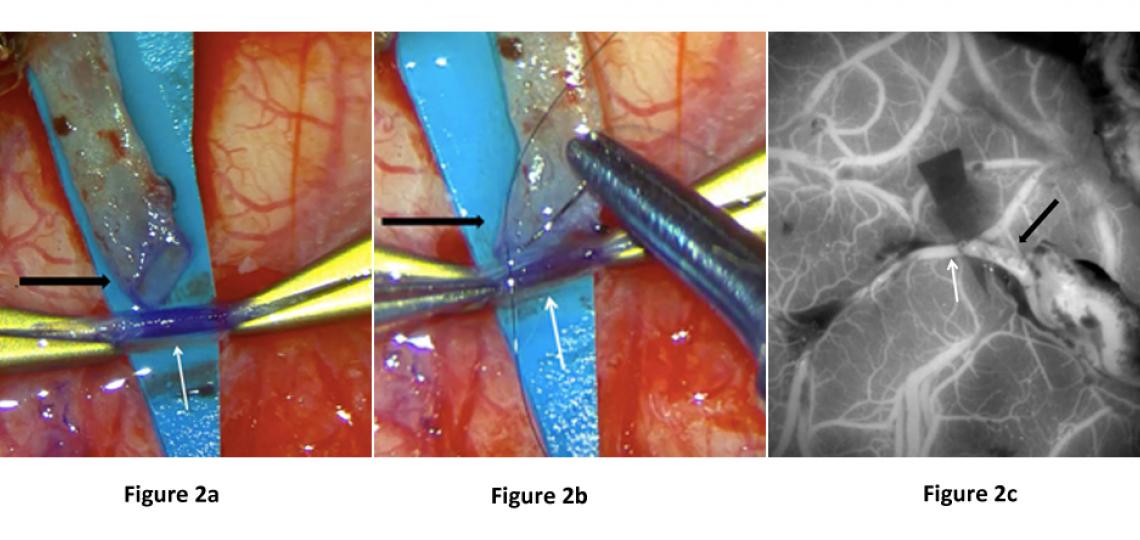
Figure 2: Images from a STA-MCA bypass surgery showing (a) the cut STA (black arrow), which has been dissected from the scalp and trimmed in preparation for use as a bypass donor, and prepared suture into the brain MCA vessel (white arrow), (b) the open end of the STA (black arrow) is being sutured onto the open MCA vessel (white arrow) and (c) intra-operative ICG dye angiogram showing blood flow through the skin vessel (black arrow) into the brain vessel (white arrow).
Indirect Revascularization
There are several variations on an "indirect" bypass that can all provide much needed increased blood flow to the brains of moyamoya patients. These strategies are all variations of each other and are very commonly performed in children where the blood vessels are small and not ideal for performing direct bypasses. The indirect procedures all similarly involve open surgery to place healthy extracranial tissues with good blood supply onto the brain's surface, and over time, they grow new blood vessels into the brain resulting in much needed supplemental blood flow. Several of the more common indirect bypass options include:
EDAS (encephalo-duro-arterio-synangiosis) - This is the most commonly performed indirect bypass procedure. Like the direct bypass, this procedure uses the superficial temporal artery (STA) from the scalp, but rather than cutting it and suturing directly to the brain blood vessels, the STA is kept intact and laid across the surface of the brain. With time, the vessel grows new branches into the brain thereby providing much needed blood flow. New blood vessel development typically takes three to six months but can continue to strengthen over years.
EMS (encephalo-myo-synangiosis) - This procedure is similar to the EDAS. However in this variation, the temporalis muscle that is naturally just above the skull near the temple is placed through an opening in the skull and onto the surface of the brain. Within three to six months, new blood supply grows from the muscle vessels to the brain vessels.
EDAMS (encephaloduroarteriomyosynangiosis) - This is a combination of the EDAS and EMS where the vessel, the dura and the muscle are laid on the surface of the brain.
Multiple Burr Holes – This procedure is most often performed in children where the young brains typically grow new blood vessels from small areas of connection with extracranial tissues through multiple small holes made in the skull.
Omental Bypass – This is a rarely used surgical strategy most often performed when all other bypass options have been exhausted. This procedure involves harvesting vascularized fatty tissue from the abdomen and tunneling it under the skin and placed onto the surface of the brain. This tissue with blood supply from abdominal vessels can similarly provide new vessel growth into the brain.
Post-Operative Care and Recovery
Surgery for moyamoya disease is best performed at specialized cerebrovascular centers like Baylor St. Luke’s Medical Center where there are expert surgeons, well trained neuro-anesthesia and specialized postoperative care in a Neurological Intensive Care Unit. Patients are typically in the hospital three to five days after surgery, are continuously hydrated and begin eating, drinking and getting out of bed the day following surgery. Patients generally have minimal hair removed during surgery.









