Our Baylor Medicine surgeons are full-time faculty at the Michael E DeBakey Department of Surgery at Baylor College of Medicine. All surgical procedures are performed at the Baylor St. Luke’s Medical Center Transplant Institute. Our surgeons tailor the transplant operation to the patient. We realize that no two patients are alike and that the operation has an important impact on outcomes.
To each case, our surgeons bring a collective experience of over 1,000 lung transplant procedures. We combine our expertise through collaboration in operative planning and case achievement. We offer all our patients the safest and most advanced comprehensive experience possible. We routinely review and accept complex cases that include patient comorbidities such as older age, prior surgeries, coronary artery disease and a variety of other unique scenarios. We tailor the operative procedure, innovations and donor selection to match the patient’s needs.
What is a Lung Transplant?
The lungs are critical for human survival and well-being. They provide vital oxygen, remove carbon dioxide, clear infectious microbes, and filter particles from the air. Our breath gives us life by allowing us to act and think.
The respiratory system consists of the upper and lower respiratory tracts. The upper respiratory tract includes the nasal cavity, paranasal sinuses, and nasopharynx. The lower respiratory tract begins at the larynx level and includes the trachea and numerous small airway branches culminating in tiny alveolar sacs. The trachea divides into the right and left main bronchi. The heart pumps blood to the heart through the pulmonary artery. This blood gets oxygenated by the lung and the oxygenated blood flows back to the heart through the pulmonary veins.
Unfortunately, the lungs are susceptible to many insults and advanced lung disease is the third leading cause of death worldwide. If a patient’s lung condition has become severe and irreversible, then a lung transplant is an increasingly viable option.
Lung transplant involves the removal of the damaged lung and replacement with a new healthy organ. To do the surgery, the doctor makes a cut in your side about 6 inches below your armpit. This cut is called an incision. Then, the doctor removes part of a rib so he or she can take out your lung a put in the new one. Next, he or she connects the new lung’s blood vessels to your body’s blood vessels and connects the main bronchial tube of the new lung to your main bronchial tube. Then the doctor closes the incision with stitches or staples. These are removed about 1 to 3 weeks after surgery. The incision will leave a scar that will fade with time.
During a lung transplant the surgeon disconnects the veins, arteries and veins and sews them to the new donor lung. After surgery, the new lung will start to work right away. You will probably spend 1 to 3 weeks in the hospital. But it may take 2 to 3 months for your energy to return fully.
Donor Procedures
Organ donation is a precious gift that we treat with the highest honor and respect. We aim to utilize the greatest percentage of offers possible while maintaining the best outcomes possible.
We have a specialized group of coordinators who receive, and review donor offers 24/7 from organ procurement organizations from around the country. We do not place restrictions on travel for consideration of organ offers, although each offer is given scrutiny to ensure the best quality possible while maintaining the greatest number of opportunities for transplant.
Our procurement team consists of surgeons and perfusionists that travel to assess and retrieve the donor’s lung. The procurement procedure involves an incision down the middle of the donor’s chest. The heart and lungs are exposed and carefully assessed. In most cases, the donor is brain dead (i.e., donation after brain death, DBD). In some cases, the donor is not brain dead, but the family has decided to withdraw care due to futility and end of life. In these cases, the donor lung can still be retrieved with a special procurement procedure termed donation after cardiac death (DCD). We have significant experience in a variety of procurement strategies, including patients with prior chest operations.
Ex-Vivo Lung Perfusion (EVLP)
The breathing lung transplant program is a mode of transplantation where the donor’s lung is kept breathing and warm, with blood pumping through it from the time of the donor procedure to the recipient implant.
This program utilizes a technology known as ex-vivo lung perfusion, which has several components that allow the lung to remain in a physiologic state throughout transportation.

The Organ Care System (OCS) is the only portable EVLP system in the world. It is the only one of two EVLP systems that have undergone a positive FDA panel review in the United States as well as two rigorous international clinical trials. In the INSPIRE trial, the most ideal standard donor lungs that were transported on OCS and transplanted were compared to those that were transported in standard ice coolers and then transplanted. Standard ice is the way that transplants have occurred for decades. Trial results suggests that those transplanted in the OCS according to protocol had a 50% in the incidence of graft dysfunction.
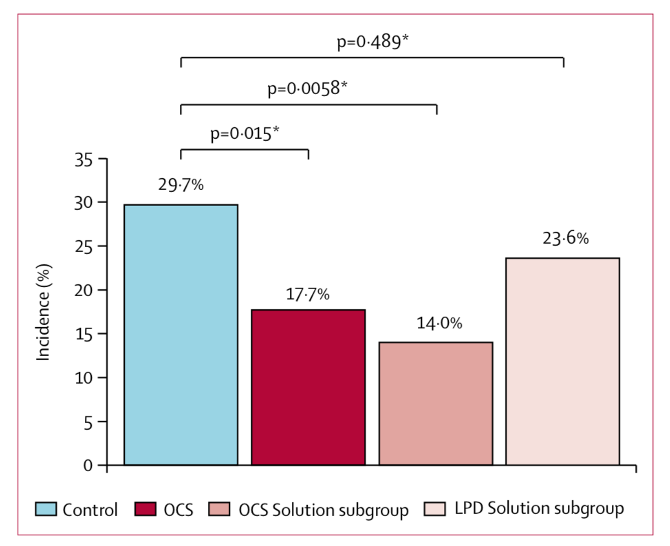
Unfortunately, it is estimated that only 5-10% of donor lung offers meet “standard or ideal conditions.” The EXPAND I trial was conducted to see the effect of the OCS on lungs outside of the ideal scenario.
EXPAND I was led by Baylor Medicine physician Gabriel Loor, M.D., along with a group of highly experienced transplant surgeons and pulmonologists from around the world. The EXPAND I results showed excellent utilization of such lungs with survival outcomes better than the national average for standard transplants. That means increasing the number of potentially transplantable organs and reducing the chance of dying while on the waitlist.
Baylor St. Luke’s Medical Center was the first site in the nation to begin the EXPAND II clinical trial and the first site in Texas to utilize the OCS lung platform. We are currently enrolling most if not all EVLP cases into the first-ever national EVLP registry TOPS (Thoracic Organ Perfusion Registry) to continue to learn about this technology and whether it should become more broadly used.
Recipient Surgery
Once the donor has been accepted, the recipient is brought to the operating room. Along with safety, patient comfort is a major objective for our team.
You will receive medicine that will allow you to relax. A breathing tube is inserted that will enable us to ventilate each lung separately during the procedure. Monitoring catheters are inserted carefully to enable us to ensure that your body and brain are receiving all the blood flow and oxygen that it needs during the procedure.
At the end of the surgery, we utilize a nerve-blocking device that cools the nerve fibers the chest wall and numbs the incision. This typically lasts for weeks after the procedure.
Type of Incisions
The type of incision depends on the type of transplant. While we generally favor double lung transplants over single lung transplants, there are many scenarios where a single lung transplant is a safer and more desirable option.
This is especially true in patients who are older with other significant comorbidities whereby a single lung transplant would allow the patient to receive a transplant more expediently and still gain the same amount of longevity as a double lung transplant.
For a single lung transplant, the incision is made under the breast fold and towards the back in the right or left. For a double lung transplant, we use an incision that spans the chest from left to right, which allows to see both lung spaces at once. The other two options include an up and down incision that we use if the patient’s anatomy is favorable for this or an isolated minimal access incision in the left and the right for the right candidate.
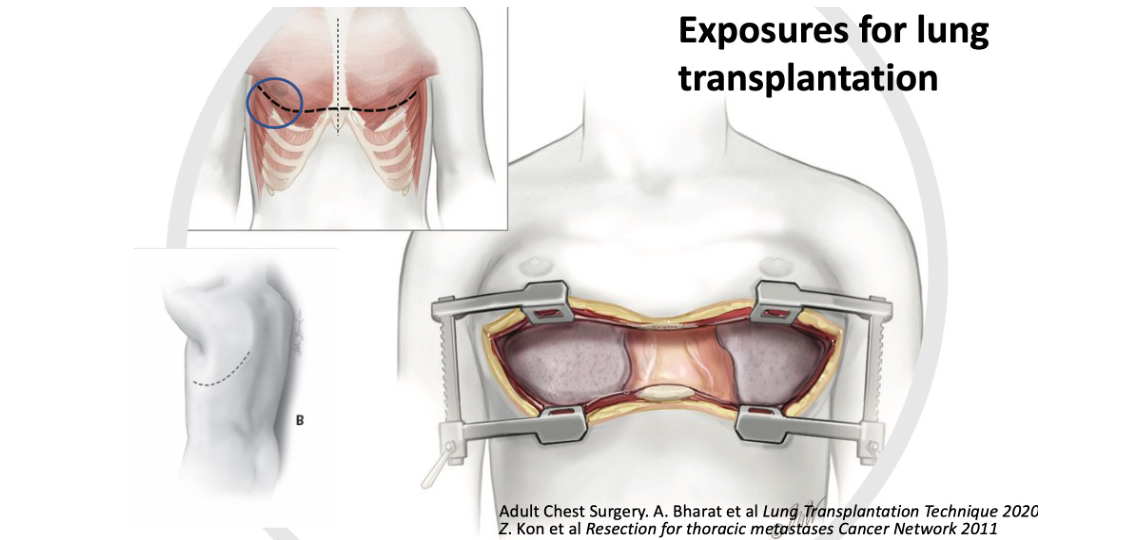
Your surgeon will review your case; your anatomy based on computed tomography images and then discuss the best approach with you prior to surgery. Once the surgeon has access to the heart and lungs, we decide whether the surgery can be done with or without cardiopulmonary support using the heart-lung machine. If we do need the heart-lung machine, we usually try to minimize the stress to the body by using a device called extracorporeal membrane oxygenation (ECMO), which provides just enough support with less inflammation.
Connections from the Lung
Next, the lung’s connections to the heart, including the pulmonary artery and vein, are identified and isolated. Once the new organ is safely near the hospital, we separate the blood vessels with a surgical sealing device. We separate the airway and remove the lung.
We have several important structures that we aim to protect but that are at risk during the surgery, these includes:
- Nerves to the vocal cords, esophagus, and diaphragm.
- Lymphatic channels that bring lymph fluid from the body to the central veins.
- The esophagus, heart, and aorta are all carefully protected throughout the procedure.
Sometimes patients have had prior surgeries or special sealant fluids like pleurodesis instilled into the chest that makes the lungs harder to extract. This may add additional time and the possibility of a greater need for a blood transfusion. Once the lung is removed, we prepare the donor lung and bring it into the chest.
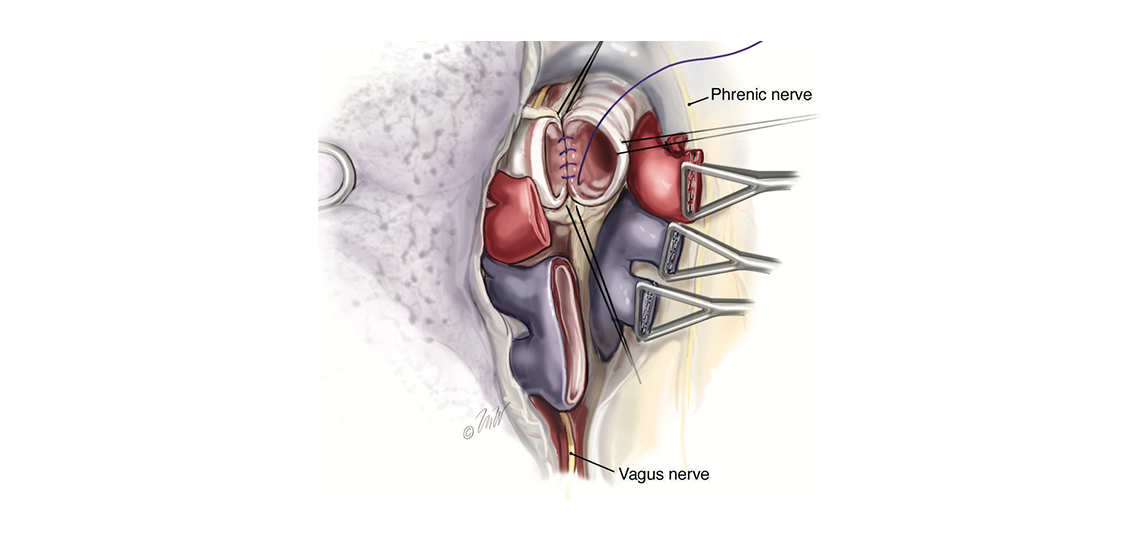
Closing Incisions
After bringing the donor lung into the chest, we sew the airway first; then we sew the pulmonary artery and the veins from the lung to the heart. We let the lungs receive blood flow and begin to ventilate. Once we complete both sides, we close the chest incision and transport you to the intensive care unit. There we will monitor closely to ensure the lungs are working well.
Potential risks that we look out for include the following:
The lungs sometimes are slow to wake up and you may require a temporary tracheostomy tube in the neck to allow you to get out of bed and perform conditioning exercises.
Bleeding is a possible complication. Occasionally there may be a need to return to the operating room to washout an area that fills with fluid from either minor bleeding or lymphatic fluid.
We monitor all organs including the heart, brain, kidneys, liver and extremities.
Throughout the process, our care teams communicate regularly with you and your family to ensure that all questions are answered as best and promptly as possible.








