Lung transplantation is an established treatment for end-stage lung disease patients. Early recognition and referral can help patients to familiarize themselves with the transplant program. We evaluate every patient on an individual basis and strive to develop a personalized path to transplantation.
Meet your Transplant Pulmonologists
Below you will find some of the most common questions.
Optimizing Your Chance of Success
In general, the better shape that a patient is in at the time of transplant, the better condition they will be after surgery. Seeking care before your disease process is too far gone is an essential first step. Then it is important to begin thinking about the requirements listed above and developing your caregiver, smoking cessation, and weight loss plans.
Pre-Condition Evaluation
At times a patient may have a condition that predisposes them to advanced lung disease; these conditions are important to recognize prior to transplant.
The most common gastrointestinal condition that predisposes a patient to advanced lung disease is gastroesophageal reflux (GERD). GERD means that food does not go down the esophagus completely and microparticles can come up and into the airways, causing inflammation. In addition, patients may have this condition after transplant. Other patients may have other esophageal disorders that makes a transplant difficult if not addressed prior to surgery.
Baylor Medicine has a comprehensive gastroenterology program that reviews your individual case and can provide guidance and treatment options ranging from minimal access surgery ahead of the transplant or procedures after the transplant to remedy your esophageal disease.
Initial Screening
Initial screening is a brief telephone interview conducted by the pre-lung transplant coordinator. We will contact your referring physician to obtain your medical records (physician evaluation notes, pulmonary function tests, laboratory tests, X-ray and chest CT scan results, lung biopsy results if available).
Initial Consultation
Transplant pulmonologists will perform a screening history and physical exam and review available physiologic studies at the initial transplant clinic visit. Patients who appear to be appropriate candidates will undergo further evaluation.
As the next step in transplant evaluation you will meet other members of our multi-disciplinary team listed below:
- Transplant Surgeon
- Transplant Coordinator
- Transplant Infectious Diseases (If applicable)
- Transplant Geriatrician (If applicable)
- Social Worker
- Financial Counsellor
- Nutritionist
- Transplant Pharmacist
The majority of these evaluations can be done as a virtual visit (telemedicine) or by telephone for your convenience. It is important that you have a designated caregiver (preferably a family member) accompanying you during the above consultations.
Outpatient Testing
All of these tests are performed on an outpatient basis. Our pre-transplant coordinator will help you schedule these tests. We will work with you to accomplish these investigations in a timely fashion. Select patients may require inpatient testing due to hospitalization with declining status. This determination will be made on a case-by-case basis by the transplant team.
List of tests performed on an outpatient basis (New Page Note: content at the end of document)
Post-Evaluation Decision
Each patient’s case will be discussed at a multidisciplinary review board the week following the completion of the evaluation. A determination will be made of the patient’s acceptability for listing, unacceptability for listing, or need for further assessment/interventions. Once approved for lung transplantation, each patient is assigned a lung allocation score based on multiple variables.
The United Network developed the Lung Allocation Score (LAS) for Organ Sharing (UNOS). The use of the LAS was designed to maximize the allocation of organs to individuals with the highest risk of death on the waiting list and the greatest benefit from transplantation. Online LAS Calculator
Waiting for Transplantation
Patients are actively listed for transplant will be routinely followed in the pre-transplant clinic until the time of their transplant. It is essential to continue exercising and pulmonary rehabilitation to be in the best physical and mental condition prior to the transplant.
The following is discussed with patients on the wait list:
Provision of contact information (office number and pager) and explanation for use. The patient’s responsibility to make him/herself available to be contacted by the transplant program at any time.
Patients are requested to inform the transplant team of any change in their circumstances, such as:
- Change in clinical status (worsening symptoms or oxygen requirements, hospitalization)
- Any changes in medication
- Vacations/travel
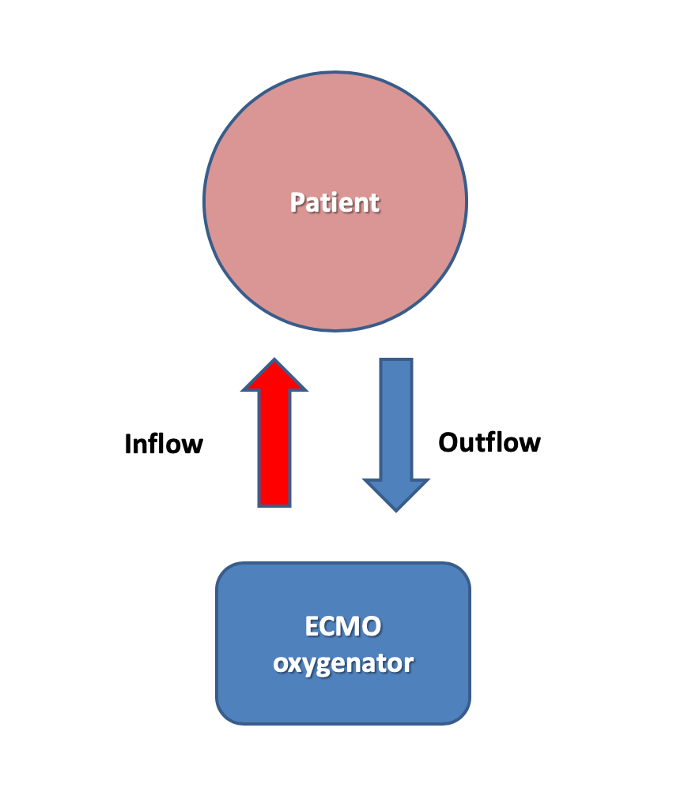
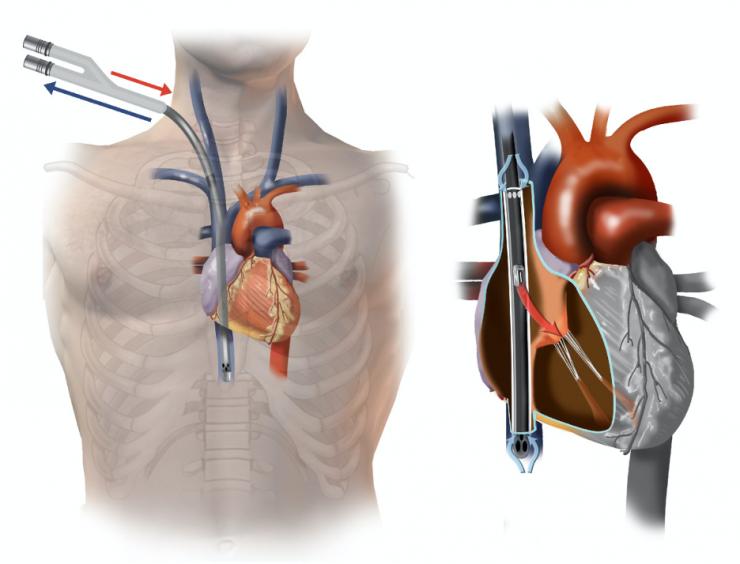
Extracorporeal Membrane Oxygenation (ECMO)
ECMO is sometimes needed for patients waiting for a lung transplant. ECMO is a device that is inserted through two large IV’s into the patient’s blood vessels and provides oxygen directly to the blood. We place ECMO lines sometimes in the upper body in a way that allows the patient to move around and remain conscious; this allows the patient to stay conditioned prior to transplant. ECMO may also be used during the transplant or afterward if the lungs take time to function normally.
While the waitlist at Baylor St. Luke’s Medical Center is lower than the national average, ECMO is an important adjunct for patients who become very sick quickly. Without an ambulatory ECMO Program, it can be difficult or impossible to bridge a patient who is critically ill to a lung transplant; many times, the ventilator support alone is not enough.
Periodical Medical Testing
You will be followed in the pre-lung transplant clinic at regular intervals. The clinic visits will involve blood work, breathing tests, six-minute walk tests, chest x-rays or chest CT scan.
Pulmonary Rehabilitation
Pulmonary rehabilitation is very beneficial in improving your condition prior to transplant. It involves a formalized program where you exercise your muscles and your breathing while being monitored. At times, these programs can improve your breathing capacity.








 Credit
Credit