What You Need to Know About Stroke
Stroke is the leading cause of long-term disability and preventable disability in the United States. It is also the fifth leading cause of death, killing nearly 130,000 people in the U.S. each year. The cerebrovascular neurosurgeons and stroke neurologists at Baylor Medicine specialize in the diagnosis and treatment of brain blood vessel disorders, including acute ischemic strokes.
If you or someone you know is having symptoms of a stroke, seek medical attention and call 911 immediately!
What Is an Ischemic Stroke?
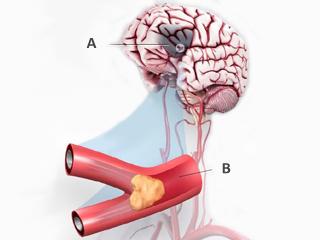
The word “ischemia” means lack of blood flow to an organ of the body. Ischemic strokes happen when a blood vessel in the brain is suddenly blocked causing lack of blood flow to that area of the brain (Figure 1).
The disruption in blood flow deprives the brain of the crucial oxygen and nutrients it needs to survive. Within minutes, the parts of the brain supplied by that blood vessel begin to suffer and to stop working properly.
If the blocked vessel is not re-opened, irreversible brain tissue injury and damage will happen to that part of the brain.
Symptoms
People who are having a stroke can exhibit a variety of symptoms, which can vary greatly depending on what parts of the brain are affected by the stroke. People suffering a stroke might experience speech difficulties, numbness, weakness of the arm, leg or face, paralysis, problems with vision, confusion, and even coma.
Stroke specialists have distilled this information into a helpful mnemonic to help remember the signs of someone having a stroke (Figure 2).
In an emergency, just think "FAST" and do the following:
Face - Ask the person to smile. Does one side of the face droop or is it numb? Is the smile uneven?
Arms - Ask the person to raise both arms. Can one arm not be raised upward or does one arm drift downward?
Speech - Ask the person to repeat a simple phrase like "The sky is blue." Is their reply slurred or does it sound strange?
Time - If you observe any of these symptoms, even if they go away, call 911 immediately. Check the time so that you’ll know when the symptoms started.
If you notice any of these symptoms, even if they fluctuate or disappear, seek medical attention immediately and call 911!
Spot a Stroke F.A.S.T.
Figure 2. Face drooping. Arm weakness. Speech difficulty. Time to call 911.
Diagnosis
While you are at the hospital, there are a number of tests and scans that a physician might use to evaluate your condition and establish a treatment plan suited to your needs.
- A CT (computed tomography) scan is an x-ray that doctors use to determine which part of the brain has been damaged and whether the stroke was caused by hemorrhage or artery blockage.
- An MRI (magnetic resonance imaging) scan uses radio waves and magnets to produce a more detailed image of the blood vessels in the brain. It helps identify the damage done to the brain after stroke.
- CT angiogram or MRI angiogram are able to obtain accurate pictures of the blood vessels in the neck and brain to look for blockages for causes of stroke.
Treatment
The primary goal in treating acute ischemic stroke is to preserve the healthy brain tissue that is at risk of dying due to the vessel blockage. Brain tissue can only survive a few hours without blood flow. Thus, to save the at-risk brain tissue during a stroke, the blood vessel blockage must be re-opened quickly in order to prevent permanent brain damage. There are two FDA approved tools that stroke doctors have to break up brain vessel blockage.
tPA (tissue Plasiminogen Activator)
tPA is a thrombolytic, or “clot-buster,” drug that is delivered through the patient’s vein and circulates in the blood stream to break up a blood clot that is blocking the brain vessel. Intravenous delivered tPA is approved by the FDA for the treatment of acute ischemic stroke. The drug can make a big difference, but only if it is given within a specified time frame (up to four and a half hours after symptoms begin). This is why thinking “FAST” is crucial in a stroke, or “brain attack.”
Mechanical Thrombectomy
Mechanical thrombectomy (mechanical blood clot removal) helps patients who have major brain blood vessel blockages and are at risk for the largest amount of brain injury and the worst strokes. Patients are candidates for this emergency procedure when they have a major brain blood vessel blocked and it has been less than six hours from the start of symptoms, and/or special brain scans show that no severe damage to the brain has already occurred.
The procedure is performed under light anesthesia by a specially trained neurointerventionalist. They place a lengthy catheter, or thin tube, into the femoral artery in the leg, and the catheter is guided up the artery into the brain’s blood vessels with x-ray guidance. An angiogram (x-ray image of blood vessels) is performed by injecting dye through the catheter and taking x-ray videos, which allow the doctor to find and visualize the blockage (Figure 3).
A special grasping device is placed from the catheter into the clot to grasp it and the device is used to then physically pull the blockage out of the brain restoring brain blood flow. If the vessel is opened in time, the brain can be saved from permanent damage. Stent retriever stroke procedures are safe and highly effective in selected patients even up to 24 hours after symptoms begin.

Figure 3. Images from a brain angiogram showing a large brain blood vessel blockage. Figure 3a: The blue arrows outline the internal carotid artery coursing from the neck to the brain and the red arrow show the blockage of the middle cerebral artery (MCA). Figure 3b: The same image with the skull eliminated and same red arrow showing the blockage. The blue shading shows the large area of brain not getting blood flow. Figure 3c: After opening the brain artery, the blood now flows normally. Figure 3d: The blood clots pulled out of the brain vessel (red) and the device (stentriever) used.
Recovery
Depending on the severity of your stroke, you may stay in the hospital for a few days to a few months to recover. You will likely either remain in the stroke unit or move to a rehabilitation ward. During this time, a team of healthcare professionals with specialized training manages your recovery. These individuals include:
- Doctors
- Nurses
- Clinical nurse specialists and healthcare assistants
- Therapists (physical, occupational, and speech/language)
- Dietitians
- Ophthalmologists
- Clinical psychologists
- Rehabilitation assistants
- Social workers
- Pharmacists
When it comes to recovering from a stroke, every person and each case is different. Some patients recover quickly needing with minimal assistance, while others are left with long-term disabilities. Some require different types of therapy, spending time practicing therapeutic exercises to regain skills that previously came easily to them. Others may have to learn how to work around their new limitations.
The rehabilitation process often requires patience and persistence, but our expert staff will be available to support you through it every step of the way. When it is time for you to be discharged from the hospital, your stroke team will work with you in order to determine what sort of support you will need at home. They will plan the necessary arrangements and help you ascertain any special services, aids, or equipment you might need.
Helpful Links









 Credit
Credit