What Is Endovascular Neurosurgical Oncology?
Endovascular neurosurgical oncology is the diagnosis and treatment of patients with tumors of the brain or spinal cord using minimally invasive procedures with imaging guidance.
The cerebrovascular neurosurgeons at Baylor Medicine and Baylor St. Luke’s Medical Center in Houston, Texas, specialize in endovascular neurosurgical oncology.
Cerebral Angiography
Cerebral angiogram is the most accurate way of studying blood vessels in the head and neck and provides additional information to non-invasive studies such as CT and MR angiography. During a cerebral angiogram, contrast is injected directly into the artery to outline the vessel's inside, and x-rays are taken at the same time to obtain a picture of the blood vessels. In neuro-oncology, cerebral angiography is most often used to determine the amount of narrowing in an artery or vein and the blood supply to a brain tumor. This is an invasive test, requiring the physician to insert a catheter into the femoral artery near the groin and navigate it to the arteries in the neck.

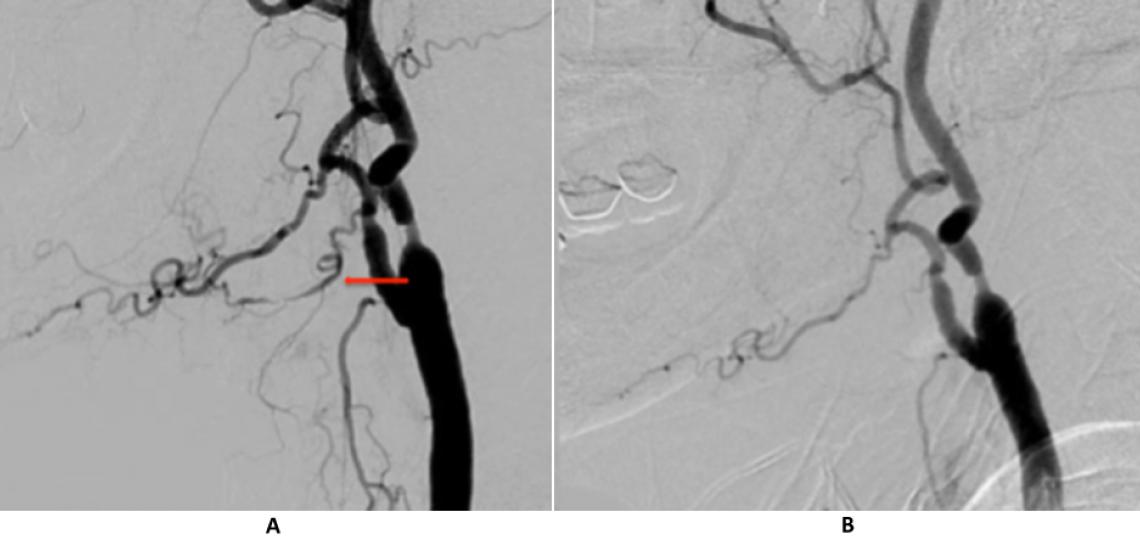
AP (A) and lateral (B) view of a right common carotid injection (normal angiogram)
Balloon Test Occlusion
Blood supply to the brain comes from four main vessels originating from the aortic arch: two vertebral arteries in the back of the neck and two carotid arteries in the front. Successful treatment of some difficult tumors at the base of the skull occasionally requires sacrifice of one of these blood vessels. Most patients tolerate this well, but in a small group of patients this can result in a potential stroke. Physicians can determine if a stroke is likely to occur with the vessel sacrifice before proceeding with surgery by doing a balloon test occlusion (BTO). During the BTO, a small and soft balloon is inflated in the artery of interest (the one considered to be sacrificed) to block the blood flow through that artery into the brain while the patient is being examined. If the other blood vessels in the neck were sufficient in supplying blood to the whole brain, the patient will remain asymptomatic. Otherwise, the patient will experience symptoms, which will be reversed with balloon deflation.

A right internal carotid artery injection with a balloon inflated in the left internal carotid artery (arrow) shows good collateral filling to the left hemisphere during a test occlusion of the left internal carotid artery.
Inferior Petrosal Sinus Sampling (IPSS)
For patients with Cushing's syndrome, IPSS can confirm a pituitary source by detecting a difference in ACTH levels in the petrosal sinus and peripheral blood samples. In addition, this diagnostic test can also help to lateralize the site of a pituitary tumor by comparing ACTH levels in both petrosal sinuses.
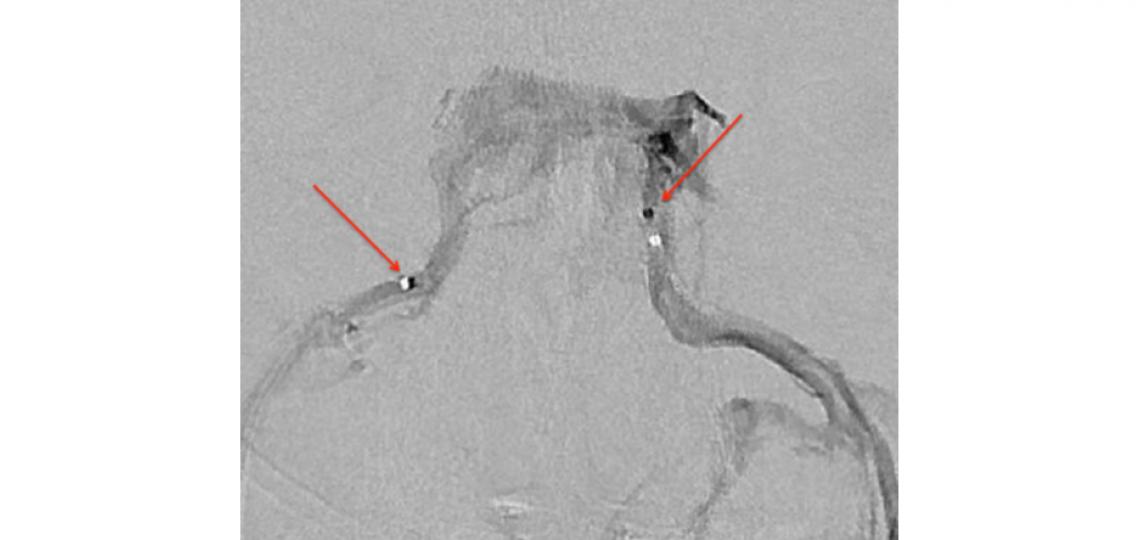
Cerebral venogram outlining bilateral cavernous sinuses and inferior petrosal sinuses. A microcatheter (arrow) is seen in each inferior petrosal sinus.
Preoperative Embolization of Brain and Spine Tumors
For certain large brain and spine (and head and neck) tumors that are very vascular, we use preoperative embolization to block the major blood supply in order to make surgical resection easier and safer by reducing blood loss. Preoperative embolization is offered as an adjunct prior to open surgery and is often performed the day before surgery. Embolization is done under biplane fluoroscopy, where a catheter is brought up through the femoral artery into the blood vessels supplying the tumor. Selective angiography of the blood vessels is then performed followed by injection of embolic material into these feeding blood vessels to reduce blood flow to the tumor.
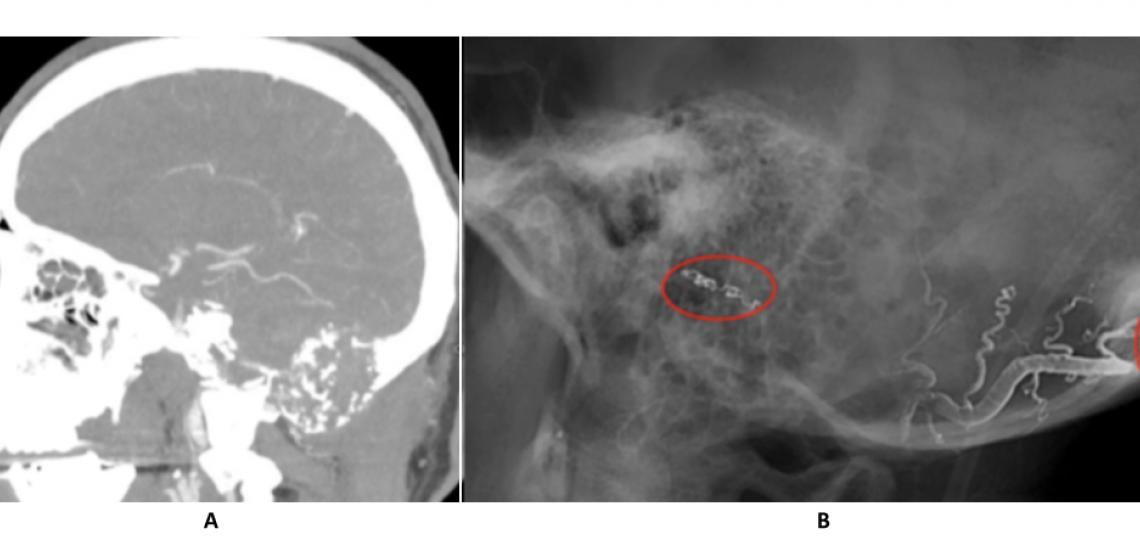
CT angiogram (A) reveals a large skull base tumor. Post-embolization angiogram (B) shows liquid embolics (onyx) in the feeding vessels supplying the tumor.
Emergent Embolization for Head and Neck Cancer
Acute bleedings due to erosion of blood vessels in the head and neck area by malignant tumors can be life-threatening. These patients often need emergent cerebral angiography to identify the source of bleeding followed by emergent embolization to obliterate the source. Embolization is performed under biplane fluoroscopy, where a catheter is brought up through the femoral artery into the blood vessels causing the active bleeding. Selective angiography of the blood vessels is then performed followed by injection of embolic material to immediately close the source of bleeding. In certain situation where there is a large defect in a major blood vessel, emergent stenting is performed to seal the defect and stop the bleeding.
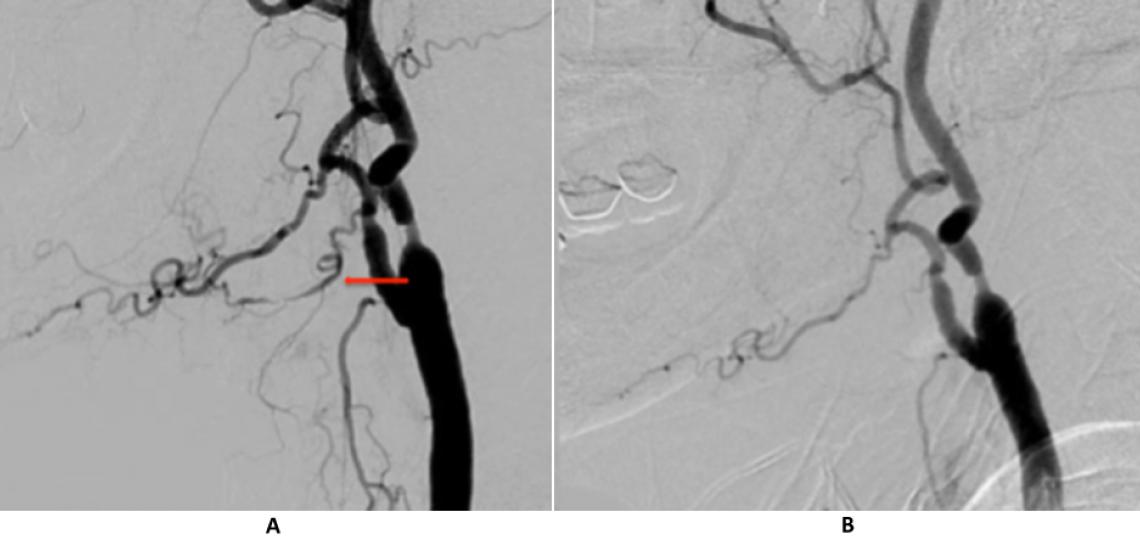
Right common carotid injection (A) shows an irregular lingual artery as the source of bleeding (arrow). The lingual artery no longer fills on the post-embolization angiogram (B).
Right common carotid injection (A) shows an irregular lingual artery as the source of bleeding (arrow). The lingual artery no longer fills on the post-embolization angiogram (B).
Intra-Arterial Chemotherapy Infusion for Retinoblastomas and Brain Tumors
Retinoblastoma is the most common childhood cancer of the eye, affecting over 300 hundred children each year in the United States. At our center, children are referred for intra-arterial infusion of chemotherapy after a multidisciplinary evaluation by the oncologic ophthalmology, pediatric oncology, and ophthalmic pathology team. Recent advances in technology and techniques allow selective chemotherapy infusion through the ophthalmic artery (the artery that supplies blood to the eye) to have over a 70 percent cure rate for advanced retinoblastoma with minimal side effects and systemic toxicity.
Our group is also in the forefront of developing advanced techniques that allow selective intra-arterial treatment into certain brain tumors through their direct blood supply. In experimental treatments, select patients with brain tumors can have chemotherapeutic agents and novel biological treatments infused directly into the arteries feeding the tumor.

An ophthalmic angiogram obtained during selective chemotherapy infusion, demonstrates the extensive angioarchitecture that allows for concentrated regional local delivery of chemotherapy.