What Are Spinal Vascular Malformations?
Spinal vascular malformations, also known as spinal arteriovenous malformations (AVMs), are the result of an abnormal connection between arteries and veins that occurs within the spinal canal or spinal dural covering. The term spinal vascular malformation includes several distinct types of vascular problems under one name. This group of spinal vascular disorders includes spinal dural arteriovenous fistulas (DAVFs), spinal arteriovenous malformations (AVMs), cavernous malformations and spinal artery aneurysms. This overview focuses on the most common types of spinal vascular malformations: spinal AVFs and spinal AVMs.
The cerebrovascular neurosurgeons at Baylor Medicine and Baylor St. Luke’s Medical Center in Houston, Texas, have specialized training and expertise in the diagnosis and treatment of spinal vascular disorders including spinal arteriovenous malformations and spinal dural fistulas. Each patient is different and our doctors provide a tailored plan for managing these often complex disorders.
Types of Spinal Vascular Malformations
Spinal Dural Arteriovenous Fistulas (Type I) - These malformations represent 70 percent of spinal vascular malformations and are the result of an abnormal connection forming between an artery and a vein in the spinal canal dural covering (Figure 1). This connection allows high pressure arterial blood to escape into the low pressure network of veins draining the spinal cord. Over time, the spinal cord is damaged by the elevated pressure. Spinal dural fistulas form spontaneously during adulthood and are not congenital or hereditary. These lesions do not rupture or bleed. They are good candidates for surgical treatment.
Spinal Arteriovenous Malformations (Type II) - Also called a glomus AVM, type II malformations consist of an abnormal connection between the arteries and veins occurring within the spinal cord itself. The connection takes place in a focused collection of abnormal vessels called the AVM nidus. These lesions represent about 20 percent of spinal vascular malformations and can present with bleeding into the spinal fluid and sudden lower extremity weakness. Treatment options depend on the location within the spinal cord.
Juvenile Arteriovenous Malformations (Type III) - These are vascular malformations consisting of an arteriovenous malformation that often involves the spinal bone, dural covering and spinal cord itself. These lesions are believed to form in early development before birth and are the most challenging to treat due to their tendency to be large, high flow and difficult to treat.
Pial Spinal Arteriovenous Fistulas (Type IV) - Pial AVFs refer to an abnormal connection between an artery and a vein on the surface of the spinal cord. They often come to attention when the vein has enlarged over time due to high pressure from the artery and begins to compress the spinal cord (Figure 2). These are rare lesions.
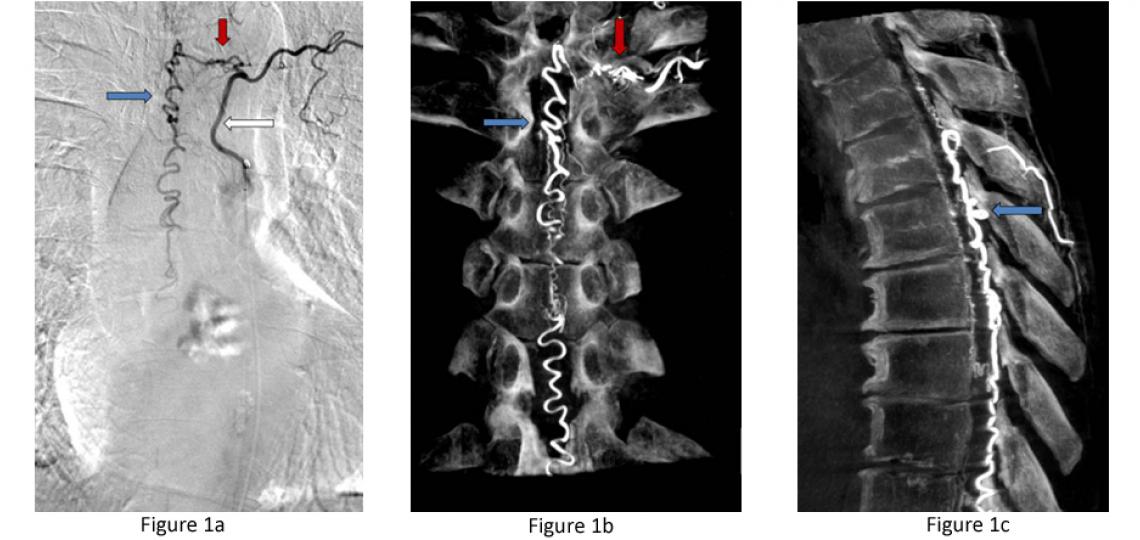
Figure 1a: Type I dural AV fistula - spinal angiogram of a left sided spinal artery (white arrow) showing an abnormal connection (red arrow) with a spinal vein that has become abnormally enlarged (blue arrow). Figure 1b: Similar view of the same fistula using a 3D flat panel CTA reconstruction showing greater detail of the abnormal artery-venous connection within in the nerve root dural sleeve (red arrow) and enlarged vein within the spinal canal (blue arrow). Figure 1c: Side or sagittal view of the same fistula showing the enlarged vein (blue arrow) along the back wall of the spinal canal behind the spinal cord.
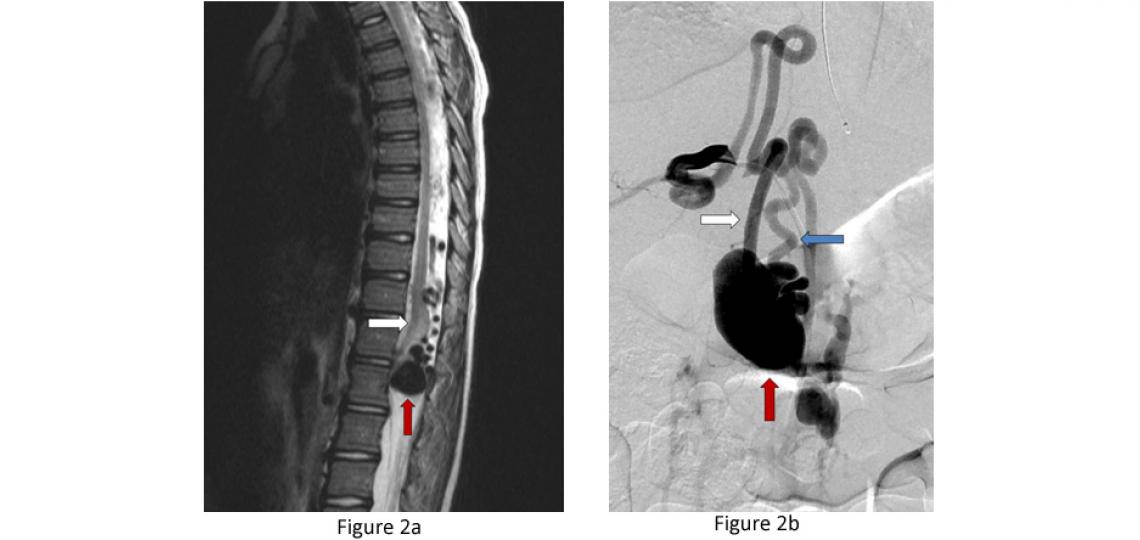
Figure 2a: Type IV pial spinal arteriovenous fistula – side view or sagittal T2 MRI of the spine showing a massively enlarged spinal vein (red arrow) compressing the spinal cord (white arrow). Figure 2b: A spinal angiogram of the same fistula demonstrating the enlarged artery (white arrow) connecting with the massively enlarged spinal vein (red arrow) and draining vein (blue arrow) leading out of the spinal canal.
Symptoms
Symptoms of spinal vascular malformations vary depending on the type of vascular problem. Detecting spinal dural fistulas (Type I) is particularly important because if left untreated, patients will slowly lose the use of their legs, but with treatment, the symptoms can be reversed. The symptoms of spinal vascular malformations can be broken into two categories: a) progressive spinal cord dysfunction and b) sudden weakness due to malformation bleeding.
Progressive Spinal Cord Dysfunction (Progressive Myelopathy) – Types I and IV
- Slowly progressive weakness in the legs over months to years
- Development of incontinence of urine
- Inability to walk long distances
- Difficulty feeling the legs
- Pain (not always)
- Impotence
Sudden Weakness or Bleeding into the Spinal Fluid – Type II
Spinal AVMs can present with sudden weakness of the legs or arms and legs.
Sudden severe back pain is can be due to a rupture of the abnormal vessels into the spinal fluid. It often happens at exactly the same time as the weakness starts. Bleeding in the spinal fluid can cause:
- Nausea
- Vomiting
- Headache
- Neck stiffness
Diagnosis
The diagnosis of a spinal vascular malformation is typically first suspected by physicians based on the patient’s symptoms. Based on the symptoms, the physician may order the following examinations:
Spinal MRI – This test is typically the first study ordered when a spinal vascular malformation is suspected. Spinal MRIs can demonstrate abnormal vessels, abnormal spinal cord changes and give important clues about the presence and location of the vascular malformation.
Spinal Angiogram – This exam is the gold standard for confirming the presence of a spinal vascular malformation, diagnosing the type of malformation (Types I – IV) and demonstrating its exact location in the spinal canal (see Figure 1).
Spinal MRA or CTA – These tests at experienced centers can demonstrate the presence of vascular malformations and can serve as a screening test. However, they provide less detailed information than a spinal angiogram.
Treatment
The appropriate management and treatment strategy varies depending on the type of spinal vascular malformation and should be carefully considered and tailored to the individual patient by a specialized cerebrovascular neurosurgeon such as those at Baylor College of Medicine Neurosurgery. The majority of cases are treated in one of two ways: surgery or embolization.
Surgery – Many spinal vascular lesions are best treated with surgery and can be cured with low risk to the patient (Type I lesions). A spinal angiogram is typically needed prior to surgery in order to guide the surgeons to the abnormal vessels. Surgery typically involves removing the posterior arch of the spinal lamina, opening the covering of the spinal canal (spinal dura) and disconnecting or removing the vascular abnormality (Figure 3).
Endovascular Embolization - Some lesions are best treated from within the blood vessels via endovascular embolization. This procedure involves advancing small tubes within the blood vessel under x-ray guidance and injecting a specially designed type of glue to close the abnormal vessel. Some lesions can be cured with embolization; other lesions may require the abnormal vessels feeding the AVM to be embolized (blocked) prior to surgery in order to make surgery safer.
Observation - Some vascular lesions are best observed rather than treated. This is typically the case with large malformations, complex malformations, asymptomatic malformations or malformations in critical areas of the spinal cord making them high risk for surgery.
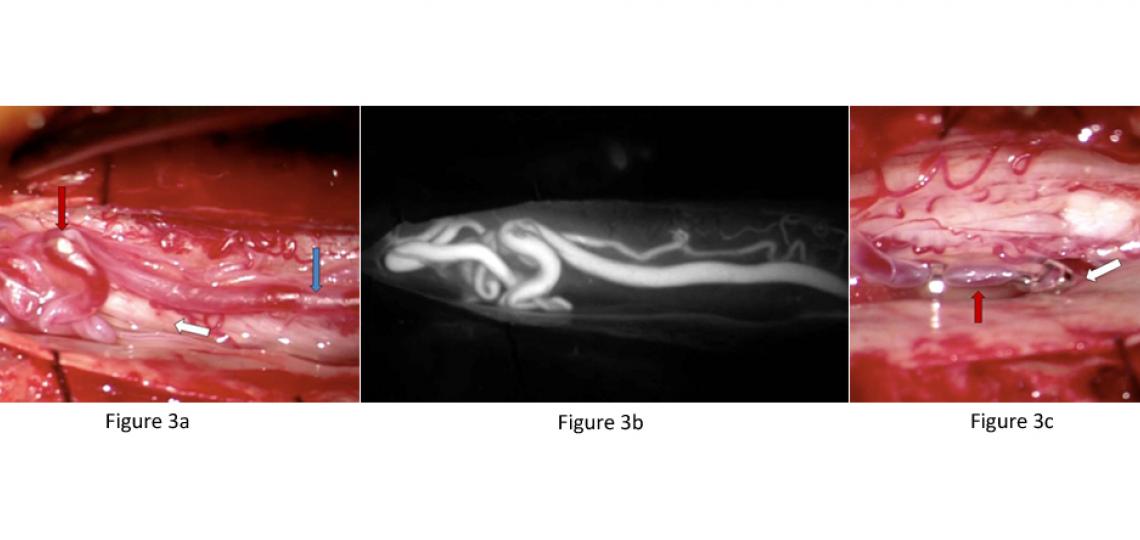
Figure 3a: Intra-operative view of a Type 1 spinal dural fistula surgery. The enlarged vein (blue arrow) laying on the spinal nerves (white arrow) is abnormally filled with red arterial blood leading to an abnormal tangle of veins (red arrow). Figure 3b: The same view of the abnormal vessels as seen with an intra-operative ICG angiogram. Figure 3c: The abnormal vein has been clipped just as it enters the spinal dura (white arrow) to stop the high arterial flow. Upstream, the vein loses its enlarged red shape and appropriately softens (red arrow) and becomes a blue-purple color like normal veins. This technique cured the fistula and the patient improved greatly.
Post-Operative Care and Recovery
Surgery or embolization for spinal vascular malformations disease is best performed at specialized cerebrovascular centers like Baylor St. Luke’s Medical Center where there are expert surgeons, radiologists and specialized post-operative care in a neurological intensive care unit. Patients are well cared for after surgery in the neurological intensive care unit by specially trained nurses and therapists to get patients out of bed and back on their feet the day after surgery.









