
Simulation-Based Learning
What is Simulation?
Seventy percent of mistakes in medicine are due to human error – not lack of medical knowledge. Simulation base training allows OB/GYN residents the opportunity to react and respond to high-risk obstetric scenarios in a life-like simulated environment so that risk to patients is substantially lowered in real-life situations.
Our Simulation Labs
Our Obstetrics Simulation Lab at Texas Children’s Hospital is a state-of-the-art facility with both low-fidelity models and two high-fidelity simulation theatres containing state-of-the-art equipment with attached control and debriefing rooms. Our high-fidelity simulation training experience includes:
- Simulation exercises on high-fidelity mannequins that mimic real emergencies to facilitate team communication, skills, and real-time responses
- Review of video-recorded simulation
- Debriefing of learners to review and discuss simulation experience
Our gynecology simulation center at Baylor College of Medicine is managed by a dedicated team of staff, including a medical director, that support independent resident/fellow simulation practice and our large-group formalized simulation sessions. The simulation center has laparoscopic trainers, open surgery simulations, and virtual reality trainers. All Baylor College of Medicine ob/gyn residents have been obtaining Fundamentals of Laparoscopic Surgery (FLS) certification for several years prior to it becoming compulsory for all ob/gyn residents nationally. Five residency classes have obtained FLS certification to date, with a 100 percent pass rate. The simulation center and guided practice sessions have been key to our success in FLS certification.



Promoting Patient Safety Through Simulation
The Department of OB/GYN has utilized simulation for many years to teach residents critical skills, teamwork, and communication in a simulated environment. Interns start their simulation-based training during orientation by being certified in the Neonatal Resuscitation Program (NRP) and learning vital intra-partum procedural skills:
- Sterile cervical exams
- Amniotomy
- Intrauterine pressure catheter placement
- Fetal scalp electrode placement
- Routine vaginal delivery skills
- Postpartum hemorrhage management
- Fetal distress management
- Intrauterine device placement
Throughout their four years at Baylor College of Medicine, our residents have three to four OB simulation training sessions per year. There is a rotating list of topics covered with emphasis and more frequent training of more common obstetrical emergencies, including:
- Postpartum hemorrhage
- Forceps and Vacuum-assisted deliveries
- Shoulder dystocia
- Amniotic fluid embolism and maternal cardiorespiratory failure
- Breech vaginal delivery
- Crisis resource management
- Teamwork and communication
- Advocacy and feedback
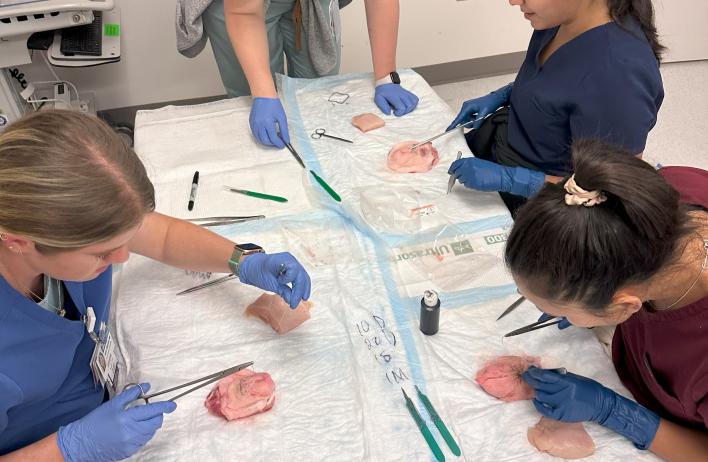
In addition to OB simulation training sessions, there are four gynecologic simulation training sessions throughout the year. These sessions focus on topics related to benign gynecologic surgery including:
- Basic and Advanced Laparoscopic surgical skills
- Cystoscopy and Vaginal Hysterectomy
- Energy sources in Surgery
- Open surgical skills
- Management of intraoperative complications
- Hysteroscopy
- Pelvic anatomy












