Introduction
The aorta is the main blood vessel that carries oxygen-filled blood from the heart to the rest of the body. It extends from the chest to the abdomen, where it branches (bifurcates) into the iliac arteries. The iliac arteries carry blood to lower parts of the body and to the legs. Sometimes with aging or other changes, a section of the aorta may weaken and begin to bulge. This bulge can enlarge over time as the walls of the aorta become thinner and stretch (like a balloon). This bulge in the aorta is called an abdominal aortic aneurysm (AAA).
An aneurysm is a bulge or balloon that forms in the wall of a blood vessel. An aneurysm is most commonly a result of an accumulation of fatty deposits on the vessel wall, but may also relate to heredity, trauma or other disease state that weakens the vessel wall. Although an aneurysm can occur in any artery of the body, it is most common in the abdominal aorta and the iliac arteries.
While the aorta’s diameter normally ranges from 2-3 cm (1 ½ inches), an aneurysm can cause it to grow to several times its normal size. Over time, if the AAA continues to grow, the aorta’s wall can become thin and lose its ability to stretch. The weakened sections of the aortic wall may become unable to support the force of blood flow. Such an aneurysm could burst, causing serious internal bleeding or even send blood clots down the legs to the feet.
Finding the Aneurysm
Unfortunately, in most cases, patients have no signs or symptoms of an AAA. During a routine physician examination, your physician may notice or feel a throbbing tender mass in the middle or lower part of your abdomen. If there are symptoms, the pain can be in the abdomen, back or chest. Some patients feel the aneurysm as a pulsating or throbbing mass in their abdomen.
Although an AAA can be discovered during a routine physical examination, most often, however, an aneurysm is found during a medical test such as a CT scan or ultrasound.
Over time, vascular disease, injury or a hereditary defect of tissue within the arterial wall can cause a weakening of the aorta. Blood pressure against the weakened area can cause ballooning (enlarging and thinning) of the aorta. Risk factors for developing an aneurysm include family history, smoking, heart disease, and high blood pressure. If you are at risk for developing an aneurysm, your physician may recommend periodic checks, which could include a physical exam and possibly a CT scan or ultrasound.
Treatment of Abdominal Aortic Aneurysm
When an aneurysm is small, physicians may recommend periodic checkups to monitor it. If an aneurysm is larger, or is rapidly growing, it has more risk of bursting or even be the cause of blood clots in the legs! There are two types of interventional treatment for AAA:
- Open Surgical Repair
- Endovascular Repair
Important Note: Not every patient is a candidate for endovascular repair. Open surgical repair and endovascular repair both have advantages and disadvantages based upon each patient’s condition and needs.
What Is an Open Surgical Procedure?
In this approach, surgery is performed to repair the section of the aorta that has an aneurysm. To reach the aneurysm, the surgeon makes a cut through the abdomen or the side of the patient. He repairs the aorta by replacing the aneurysm section with a fabric tube called a “graft” which is sewn into place and acts as a replacement blood vessel. The blood flow through the aorta is stopped while the graft is put in place. The surgical procedure is performed under general anesthesia and takes about three to four hours to complete.
Open surgical repair is a proven medical procedure that works. However, it also has a long recovery period. Patients usually stay overnight in the intensive care unit and stay another 5-10 days in the hospital. Many patients are unable to eat normally for 5-7 days after the surgery. The overall recovery period can last up to three months. As with any procedure, open surgical repair has a risk of complications.
What Is an Endovascular Repair (EVAR)?
“Endovascular” means “inside or within a blood vessel.” Your surgeon will implant this graft, which has a covered material so as to prevent blood from leaking into the aneurysm once it is properly placed in the body. Your surgeon will gain access to the large aorta (site of the AAA) via means of using both groin arteries (femoral arteries) with a percutaneous technique.
This involves entering the anesthetized femoral arteries with a needle. A small surgical incision in this area is made to allow safe passage of the student-graft into its place. Local novocain is used in almost every EVAR. General anesthesia will only be used in extremely unusual circumstances. Thus no respirator or tube in the windpipe is necessary. The repair of these arteries is done by surgical closure of these holes with pristine antimicrobial sutures and solutions. In the rare event that the arterial access sites do not close adequately, a standby surgeon picked for your specific care will then suture these holes closed.
Before Surgery
Before the procedure, your surgeon will look at pictures of your aorta (CT scan and angiography). From these pictures, an appropriate type graft as well as the correct size for each part of the AAA endovascular graft so that it will fit your blood vessels will be chosen.
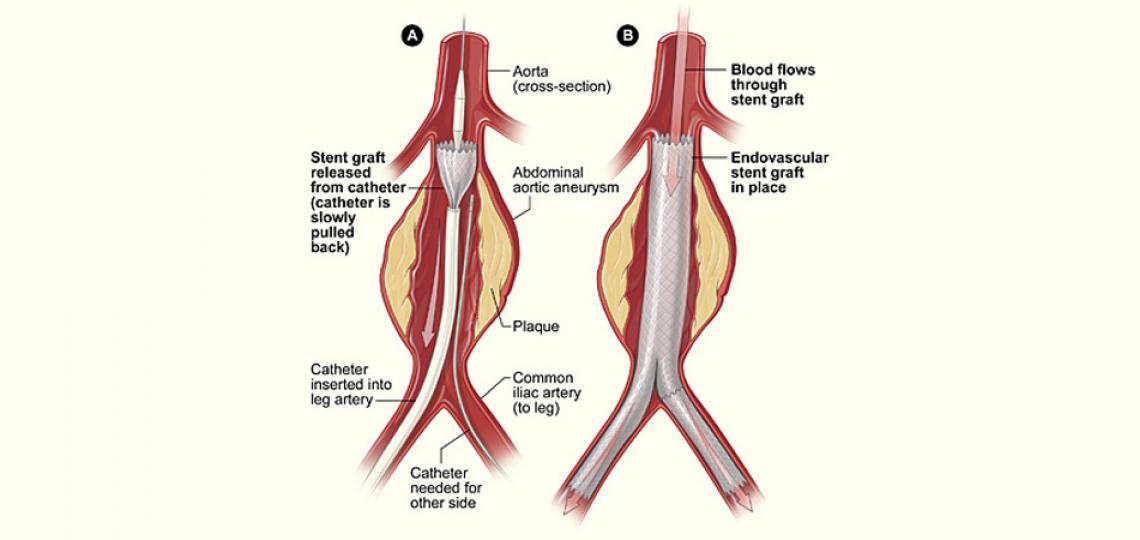
Using fluoroscopy (x-rays) for visual guidance, the delivery catheter is advanced through the large vessel in your thigh (iliac vessel) to the aneurysm site in your abdomen.
A stent graft (fabric tube) is inserted into the arteries and positioned inside the aorta, which seals off the aneurysm from the circulation). The graft makes a new path through which the blood flows.
After Surgery
After expansion of the stent graft, the delivery catheter is withdrawn and removed, leaving the stent graft within the vessel. Depending on the shape and size of your aneurysm, additional stent grafts may be placed to ensure that the aneurysm is completely excluded. x-rays and/or intravascular ultrasound imaging procedures are performed to verify that the stent graft is properly placed within the aneurysm.
The endovascular graft remains inside the aorta permanently through the use of metal prongs, or anchors as well and/or a tight fit (radial force) against the wall of the aorta.
Before the procedure is finished, x-rays will confirm that the blood in the aorta flows through the graft, not through the aneurysm. The area in each leg will be closed with a few stitches.
In one percent of the cases, it will be necessary to have a surgeon perform this part of the procedure if the holes do not close with the percutaneous technique. There will always be a surgeon as stand by assigned to your particular case.
Benefits of an EVAR
Endovascular repair typically takes about three hours to complete. This will result in less discomfort, a shorter hospital stay and faster recovery as compared to the open surgical technique. You will typically have a hospital stay of only one or less likely two nights.
You can usually return to normal activity within one to two weeks after the procedure. You will lose less blood and are less likely to need a blood transfusion while in the hospital. You are able to drink and eat sooner whereas and bowel function returned to normal sooner. You are able to walk sooner, and be discharged from the hospital sooner.
Endovascular repair also will require:
- Routine CT scan or MRA at predetermined intervals
- Routine visits with your physician
In about one to three percent of patients, there is also a possibility that additional treatment or surgery may be required after the initial endovascular repair. This can occur if the body creates new blood vessels that continue to feed the original AAA so called endoleak. Though there are various forms of endoleak, these are only treated if the aneurysm appears to be enlarging over time.
Are You a Good Candidate for an EVAR Procedure?
Requirements should include:
- Be 18 years of age or older
- Not be pregnant
- Be sufficiently healthy to undergo a 2-4 hour implantation procedure
- Be available to attend regularly scheduled office visits following the procedure, including radiographic imaging studies to evaluate the status of the graft and aneurysm.*
*Imaging studies may be required as often as every three months or as infrequently as every 12 months, depending on the status of your aneurysm and graft for up to five years after implantation.
Patients having very large aneurysms and/or aneurysms or vessels that are much more angled may not be good candidates for endovascular treatment.
What Grafts Are Available?
Cook Zenith Stent Graft. The Zenith AAA Endovascular Graft is made up of three parts: a “main body” and two “legs.” The main body is positioned in the aorta. The legs are positioned in the iliac arteries and connect to the main body. The graft thus extends from the aorta below the renal arteries (kidneys) into both iliac arteries.
The graft itself is made of a polyester graft material like that used in open surgical repair. Standard surgical suture is used to sew the graft material to a frame of stainless steel stents. These self-expanding stents provide support. The graft has several gold marks to help the doctor see the device during placement. All of these materials have a long history of use in medical implants.
Medtronic Endurant Stent Graft. The Endurant Endovascular Graft is made up of two parts: a “main body with one leg attached” and a contralateral leg segment. The stent graft, which is woven polyester tub (graft), is covered by a tubular metal web (stent) and is sewn together at many points.
The main body with leg attachment is positioned in the aorta. The contralateral extension is positioned in the iliac artery. There is a fixed section where the graft attaches above the kidney arteries to prevent the graft from moving (migration). The graft thus extends from the aorta below the renal arteries (kidneys) into both iliac arteries.
Gore Excluder Stent Graft. The endovascular graft is a two-piece, bifurcated graft that lines the aorta and extends from below the renal (kidneys) arteries into both iliac arteries. It is made up of an ePTFE (expanded polytetrafluoroethylene) covering with an outer metallic support structure known as a stent.
The main body with leg attachment is positioned in the aorta. The contralateral extension is positioned in the iliac artery. The graft thus extends from the aorta below the renal arteries (kidneys) into both iliac arteries.
Endologix AFX Stent Graft. The graft itself is made of an ePTFE (expanded polytetrafluoroethylene) over a Nitinol framework skeleton. It is unique in that it has a unibody-bifurcated design for delivery from the main side with a large introducer and from the opposite leg with a very small introducing sheath.
Trivascular Ovation Stent Graft. At 14F OD, the Ovation Prime Abdominal Stent Graft System is the lowest profile AAA endograft system, offering enhanced deliverability — even through narrow and tortuous anatomies. It has a trimodular design with suprarenal stent fixation. The size has been decrease to use without a sheath for insertion.
Upon deployment, integrated polymer-filled sealing rings are expanded to exactly conform and seal to the patient’s unique anatomy, excluding the aneurysm.
Immediately afterwards, you may need to lay flat for 2-6 hours to allow the leg wounds to begin healing. Patients have reported feeling discomfort for the first few days following the procedure in the groin areas as the anesthetic wears off. You may experience side effects such as swelling of the upper thigh, numbness of the legs, nausea, vomiting, leg pain or throbbing, malaise, lack of appetite, or fever. You will be given appropriate medications to take home which will include antibiotics.
Why Follow-Up Is Extremely Important
It is possible for problems to occur that do not cause noticeable symptoms. Therefore, your doctor needs to look at pictures (x-rays, CT scan) of your aneurysm and graft on a regular basis. Though extremely rare, if a problem occurs, your doctor may need to recommend additional procedures.
Some problems that might occur are listed below:
Endoleak. An endoleak occurs when blood from the aorta continues to leak into the abdominal aneurysm. Most endoleaks do not require treatment. However, a small number require further treatment.
Graft movement (migration). Because blood vessels can change over time with aneurysm disease, it is possible for a graft to shift position over time. Because graft movement cannot be felt, it is important to keep your routine follow-up visits with me. Graft movement, if it occurs, can be seen with a CT scan.
Aneurysm growth or rupture. Symptoms of aneurysm growth are not always present. Symptoms may include pain, numbness or weakness in the legs
Limb (leg artery) occlusion. Symptoms of this invariably include leg or hip pain during walking, leg discoloration, or leg coolness.
Recommended follow-up may include check-ups or x-ray testing at:
- 1-3 months
- 6-12 months
- Yearly thereafter
There is a rare risk of allergic reactions related to the contrast dye used in the CT scan. Talk with your surgeon if you have any concerns regarding these exams.
These exams should be considered a long-term commitment to your health and well-being. They are necessary to evaluate your treatment and any changes over time. Additional evaluations based on findings at the follow-up visit may be required.
You should also call if you are required to reschedule your follow-up visit for any reason.
The risks and benefits of the endovascular graft and procedure which you may want to discuss with your physician include:
- Risks and differences between endovascular repair and open surgical repair
- Potential advantages of traditional open surgical repair
- Potential advantages of endovascular repair
- The possibility that additional endovascular treatment or surgery may be required after initial endovascular repair
— Produced by Dr. Neil Strickman








