DeBakey Research Awards 2023
The Michael E. DeBakey Excellence in Research Award recognizes scientists whose recent research demonstrates the breadth and depth of basic science at Baylor College of Medicine. The awards are given on an annual basis in recognition of Baylor faculty who have made the most significant published scientific contribution to clinical or basic biomedical research during the past three years. Awardees receive a commemorative medallion and fund to support their research. The awards are funded by the DeBakey Medical Foundation.


Fritz Sedlazeck, Ph.D.
Associate Professor at the Human Genome Sequencing Center, Baylor College of Medicine
Associate Professor at the Department of Molecular and Human Genetics, Baylor College of Medicine
Adjunct Associate Professor at the Department of Computer Science, Rice University
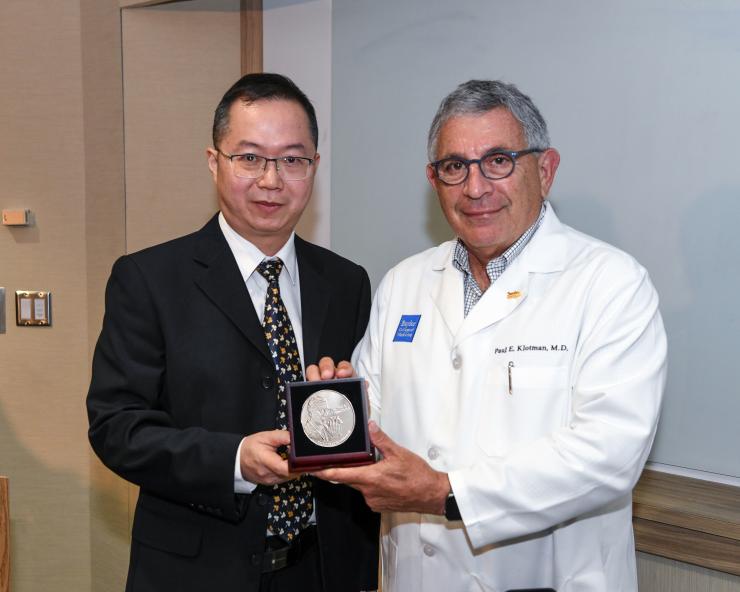
Yong Xu, M.D., Ph.D.
Professor, Associate Director for Basic Sciences
USDA/ARS Children's Nutrition Research Center, Department of Pediatrics
Section of Endocrinology, Diabetes, and Metabolism, Department of Medicine
Department of Molecular and Cellular Biology
Baylor College of Medicine

François St-Pierre, Ph.D.
Assistant Professor of Neuroscience and Biochemistry and Molecular Biology
McNair Scholar

Jeffrey Rogers, Ph.D.
Human Genome Sequencing Center and Department of Molecular and Human Genetics
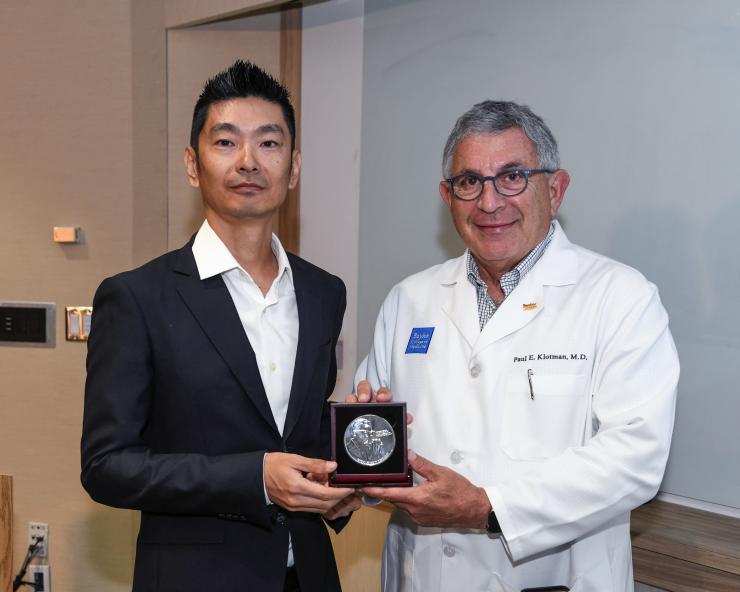
Daisuke Nakada, Ph.D.
Professor
Department of Molecular and Human Genetics

Olivier Lichtarge, M.D., Ph.D.
Cullen Foundation Endowed Chair and Director,
CIBR Center for Computational and Integrative Biomedical Research
Professor of Molecular and Human Genetics, and
Biochemistry and Molecular Pharmacology








