What is pulmonary embolism?
Pulmonary embolism is the sudden blockage of a major blood vessel (artery) in the lung, usually by a blood clot. In most cases, the clots are small and aren't deadly, but they can damage the lung. But if the clot is large and stops blood flow to the lung, it can be deadly.
What causes pulmonary embolism?
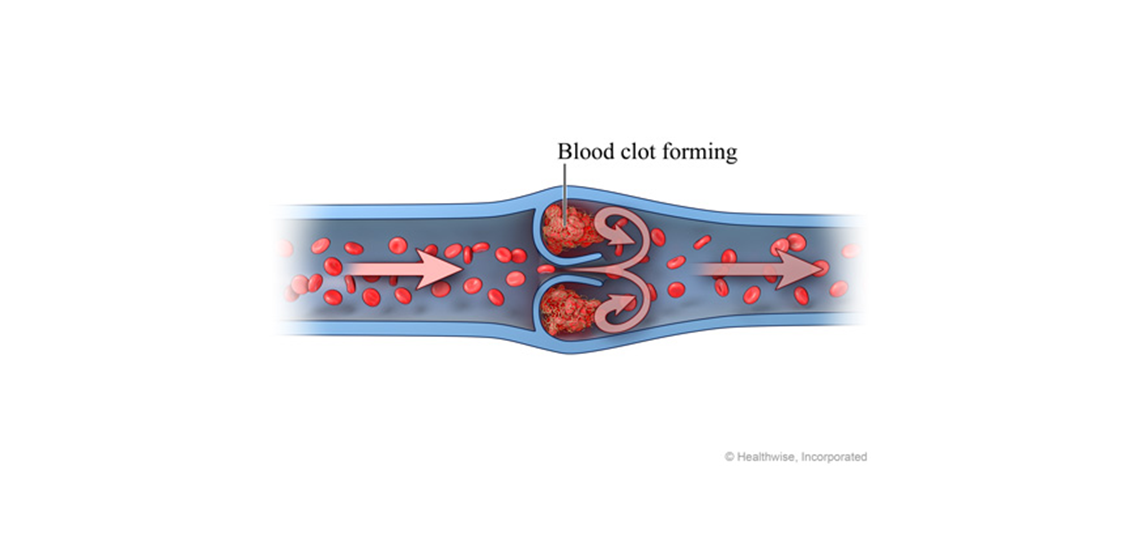
Pulmonary embolism is caused by a blocked artery in the lungs. The most common cause of such a blockage is a blood clot that forms in a deep vein in the leg and travels to the lungs, where it gets lodged in a smaller lung artery.
Almost all blood clots that cause pulmonary embolism are formed in the deep leg veins. Clots also can form in the deep veins of the arms or pelvis.
Sometimes blood clots form in surface veins. But these clots rarely lead to pulmonary embolism.
In rare cases, pulmonary embolism may be caused by other substances. They include:
- Small masses of infectious material.
- Fat. It can be released into the bloodstream after some types of bone fractures, surgery, trauma, or severe burns.
- Air bubbles or substances that get into the blood from trauma, surgery, or medical procedures.
- Tumors caused by rapidly growing cancer cells.
- Amniotic fluid.
What increases your risk of pulmonary embolism?
Anything that makes you more likely to form blood clots increases your risk of pulmonary embolism. Some people are born with blood that clots too quickly. Other things that can increase your risk include:
- Being inactive for long periods. This can happen when you have to stay in bed after surgery or a serious illness, or when you sit for a long time on a flight or car trip.
- Recent surgery that involved the legs, hips, belly, or brain.
- Some diseases, such as cancer, heart failure, stroke, or a severe infection.
- Pregnancy and childbirth (especially if you had a cesarean section).
- Taking birth control pills or hormone therapy.
- Smoking.
You are also at higher risk for blood clots if you are an older adult (especially older than 70) or extremely overweight (obese).
What are the symptoms of pulmonary embolism?
The most common symptoms of pulmonary embolism are:
- Sudden shortness of breath.
- Sudden, sharp chest pain that's worse when you cough or take a deep breath.
- A cough that brings up blood or pink, foamy mucus.
Pulmonary embolism can also cause more general symptoms. For example, you may:
- Feel anxious or on edge.
- Sweat a lot.
- Feel lightheaded or faint.
- Breathe fast.
- Have a fast heart rate or palpitations.
Signs of shock may be another symptom.
If you have symptoms like these, you need to see a doctor right away, especially if they're sudden and severe. Quick treatment could save your life or reduce the risk of future problems.
How is pulmonary embolism diagnosed?
It may be hard to diagnose pulmonary embolism. That's because the symptoms are like those of many other problems, such as a heart attack, panic attack, or pneumonia.
A doctor will do a physical exam and ask questions about your past health and your symptoms. This helps the doctor decide if you are at high risk for pulmonary embolism.
Based on your risk, you might have tests to look for blood clots or rule out other causes of your symptoms.
Tests that are often done if you have shortness of breath or chest pain
- A chest X-ray. Results may rule out an enlarged heart or pneumonia as a cause of your symptoms. If the chest X-ray is normal, you may need other tests.
- Electrocardiogram (EKG, ECG). The electrical activity of the heart is recorded with this test. EKG results will help rule out a possible heart attack.
Other tests
- D-dimer. This blood test measures a substance that is released when a blood clot breaks up. D-dimer levels are usually high in people with pulmonary embolism.
- CT (computed tomography) scan or CT angiogram. These tests might be done to look for pulmonary embolism or for a blood clot that may cause it.
- Magnetic resonance imaging (MRI). This test may be used to view clots in the lungs.
- Doppler ultrasound. This test uses reflected sound waves to look for a blood clot in the large veins of the legs.
- Echocardiogram (echo). It finds abnormalities in the size or function of the heart's right ventricle, which may be a sign of pulmonary embolism.
- Ventilation-perfusion scanning. This test scans for abnormal blood flow through the lungs after a radioactive tracer has been injected and you breathe a radioactive gas.
- Pulmonary angiogram. This invasive test is done only in rare cases to diagnose pulmonary embolism.
How is pulmonary embolism treated?
Doctors usually treat pulmonary embolism with medicines called anticoagulants. They are often called blood thinners, but they don't really thin the blood. They help prevent new clots and keep existing clots from growing.
Most people take a blood thinner for a few months. People at high risk for blood clots may take it for the rest of their lives.
If symptoms are severe and life-threatening, "clot-busting" drugs called thrombolytics may be used. These medicines can dissolve clots quickly, but they increase the risk of serious bleeding. Another option is surgery or a less invasive procedure to remove the clot (embolectomy).
Some people may have a filter put into the large vein (vena cava) that carries blood from the lower body to the heart. A vena cava filter helps keep blood clots from reaching the lungs. This filter might be used if you have problems taking an anticoagulant.
© 2016-2020 Healthwise, Incorporated.








 Credit
Credit